Valiant office practise
Boost your office practise with the lasted updates from this exclusive issue
Telementoring!
Do “mentoring” right from your office! Welcome to the world of Proxiemie
We all remember our first complex case. Despite meticulous planning, we brought our trusted senior colleague for ‘just in case’ scenarios. What if, your trusted colleague can still guide you while sitting in their airconditioned office?

Proxiemie are bringing in their virtual reality programme with a function called telepresence. You can attend and teach live surgeries while sitting in your clinic. The software works with any hardware and all you need is a laptop to give instructions.

They also make proprietary kits for wearable cameras and dedicated tablets and cameras. For Surgeons in the West, it is GDPR and HIPAA compatible.
‘Telementoring’ as they say, can improve skills and experience beyond geographical barriers like the instance where the surgeon sitting in his living room in Seattle, virtually scrubbed in to guide surgery in London.
Should Plaster of Paris be called “Plaster of PARIS”?
Have you ever wondered why they call it Plaster of Paris?
Well, it’s got a pretty cool backstory! Picture this: King Henry III was visiting Paris in 1254, and he saw these super impressive white walls. He thought they were so awesome that he decided to bring the same plastering technique back to England. And just like that, it became known as the plaster of Paris! Two military surgeons Nikolay Ivanovich Pigarov, a Russian and Anthonius Mathijsen, Dutch are classically considered as the ones who started the use of plaster of Paris for treating fractures.
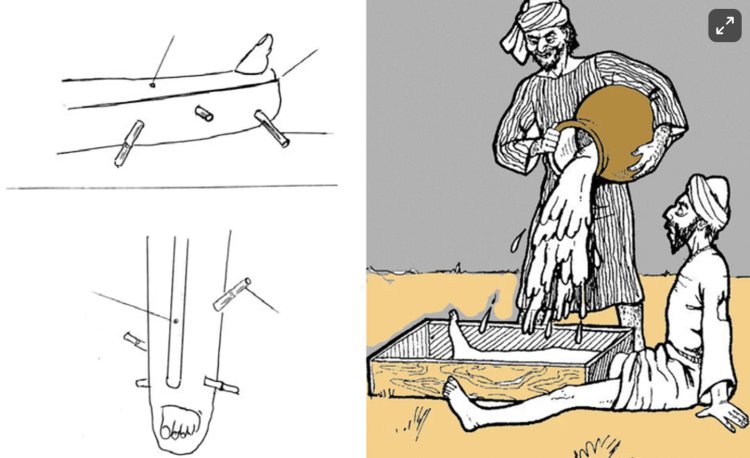
Now, that’s the usual story everyone knows, but there’s a cool claim from Raoufi that the same process of purifying gypsum was used in ancient Persia. There’s this fascinating tale mentioned by Zeinoddin Vasefi in his 16th-century book. It’s about a prince who got beaten up by a wrestler in a play. The court physician, Ostad Sheik, made him sit on the ground, dug a hole, set his fractured leg, and poured “Doughaab” (which is a gypsum and water mix) over it. After about 40 days (about 1 and a half months), the prince’s leg was all healed up!
And get this, William Eaton, an English diplomat, saw gypsum being used to treat fractures with linen dressings and was so amazed that he wrote to his friend Mathew Guthrie about it, complete with detailed drawings.
So, what do you think? Should we call it the plaster of Paris or the plaster of Persia?

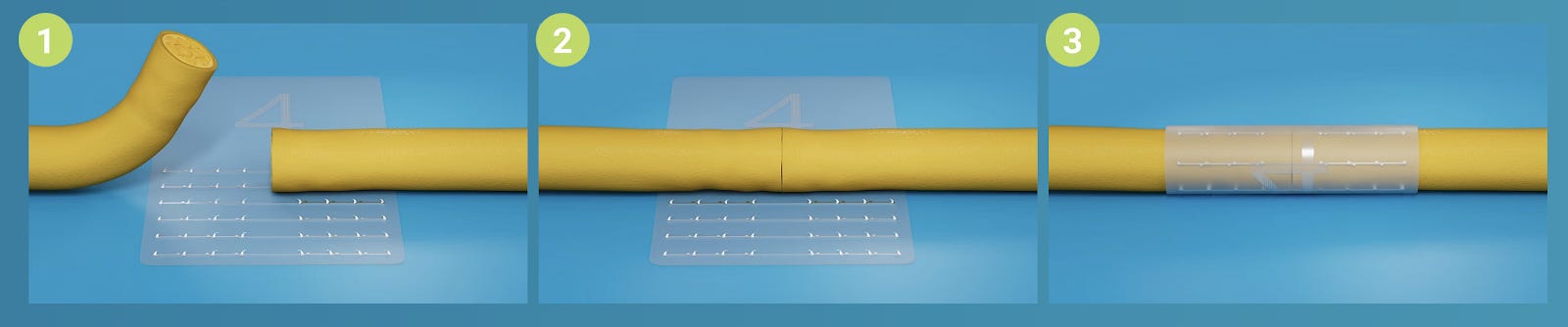
Being valiant with WALANT: #SurgicalPearl:
WALANT is a revolutionary procedure that helps us cut costs and increase office orthopaedic practice. Let us look at ten tips for effective WALANT by Degreef et al
(1) Choose indications wisely.
(2) Prepare the syringe and drugs - long 30G needle, lidocaine 1% - bicarbonate buffered
(3) Mark the needle entry point proximal to the operation field.
(4) Introduce the needle 90° in the skin by pinch injection and inject a 0.5 mL visible bleb.
(5) Use both hands: one on the syringe and one to stabilize.
(6) Progress from proximal to distal.
(7) Blow before you go.
(8) Avoid large nerves by keeping a 5 mm distance and awareness (ultrasound optional).
(9) Second needle prick, if needed, within the 1 cm margin of palpable tumescence.
(10) Wait 30 min before incising.

PRP in ARCS: #InTrials
Is PRP useful in rotator cuff surgeries? Should we give it post-operatively during office visits? All these questions linger in our minds.
Ben Liu et al in their recent RCT, tried to answer these questions. The trial involved 58 patients who underwent arthroscopic rotator cuff repair (ARCR) with PRP augmentation. Half of these patients received an additional PRP injection two weeks after surgery, while a control group received no PRP treatment.
The results were promising, especially for patients with larger tears (>2 cm). Those who received PRP during surgery had a significantly higher rate of successful healing and reported less pain and greater satisfaction compared to those who did not receive PRP. The extra office injection did not however make a difference.

Combo Offers! #MostCited
Caudal epidural steroid (CES) injection is a first-line intervention for patients suffering from lower lumbar radiculopathy not responding to other conservative measures. You can do it in three different ways - fluoroscopy-guided or USG-guided or using the combo of both USG and fluro.
Lee et al. analyzed the mid-term efficacy and safety with the use of all three modalities for CES injection. 154 patients were analysed retrospectively.
Key takeaways:
-
No difference in injection success rate or functional outcomes.
-
Least time for injection - Combo group
-
Easy identification of blood vessels - Combo or USG-guided group
-
Less chance of intravascular injection - Combo Group
Opt for a combo method wherever possible.

Events to check out:
-
12th Emirates International Orthopaedic Congress 15 – 17 Nov 2024 Abu Dhabi, UAE
-
German Spine Congress – 19th Annual Meeting of the German Spine Society 27 – 29 Nov 2024 Hamburg, Germany
-
Rome International Shoulder Course. The Experts question themselves. VIII Edition 30th Nov 2024 Rome, Italy
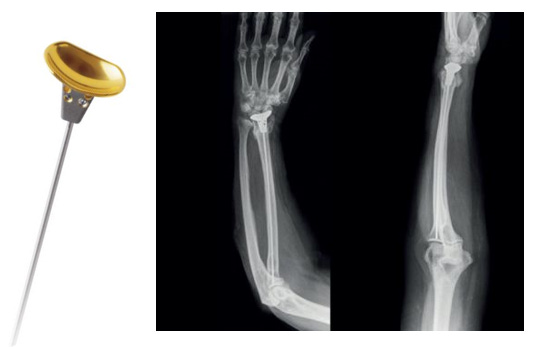
Answer to last month’s question:
Which of the following methods of proximal humerus reconstruction has the lowest 5-year survival rate after tumour excision?
-
Modular prosthetic reconstruction
-
Reverse shoulder replacement
-
Osteoarticular allograft reconstruction
-
Allograft prosthetic complex reconstruction
According to a systematic review of 752 patients by Aiba et al, Osteoarticular allograft reconstruction had the lowest 5-year survival rate when compared to other procedures.
Question of the month:
Have a surgical September folks. Seeya next month