The art of seeing the unseen
Enjoy reading this special issue of #MSKRadiology

No more “move C-arm, Shoot!” #NeoArmory:
One way to keep your Gas-Man happy is definitely to take fewer C-arm shots. The happiness of your Gas Man is directly proportional to doing more cases (seriously). But do fewer C-arm shots mean going in blind? It doesn’t have to be…
We welcome TRACKX to the stage. This NC-based company has developed a simple plug-and-play universal instrument tracking technology. You just have to attach the disposable kit to your C-arm and it provides real-time virtual live fluoro images (without shooting X-rays) and automatically recalibrates with every shot. Of course, your instrument has position sensors attached to it. An excellent video to show the workflow.
The sensors (Snaps) are available as universal or as tailor-made for a particular company. Currently, percutaneous pedicle screws are covered, but trauma implants are in the line.

They claim that this tech can reduce the number of X-rays by 74.8%, radiation exposure by 91.8%, and OR time by 56 minutes (MIS-TLIF). Another study shows instrument tracking an average of 5.69 minutes, 14 C-arm images, and 7.89mGy are saved. It’s more impressive when you realize these numbers are for a single screw.

At a time when mixed reality is the new fad, simpler tech that can overlay onto the existing infrastructure is actually what we need now.

Absorptiometry over years - #FromTheHistory:
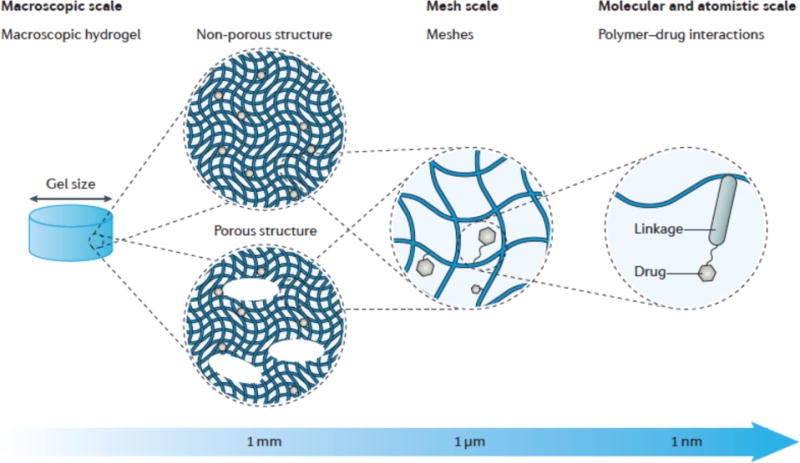
Measuring Bone Mineral Density (BMD) and defining osteoporosis have not always been as easy as we are today. Let us look at the development of the present-day Dual Energy Xray absorptiometry scans.
In the earlier days, bone densities were quantified by visual comparison with the density of known objects. A significant milestone was the development of Single Photon Absorptiometry (SPA) in 1963 by Cameron and Sorensen. This method used radioisotopes like I-125. The patient has to immerse his peripheries in the water bath to provide a uniform path for gamma rays. The bone density was calculated by subtracting the photons attenuated by soft tissues from the photons attenuated by bone and soft tissue together. SPA could only measure the peripheral bone densities. To measure the axial bone densities, Madeson et al described Dual Photon Absorptiometry where gamma rays of 2 different photon energies were used. BMD was calculated using algebraic equations. You may note that these methods need costly and hazardous radioactive substances to calculate BMD.
In the Osteoporosis Update conference in San Francisco, Jay Stein for the first time presented the technique of Dual Xray absorptiometry where the gamma rays of DPA were replaced by X-rays. The concept of DXA was so unbelievable the course chair Harry exclaimed,
Where is the catch? Jay. Jay replied, “There is no catch here”
With the support and standardizations from the International Society of Clinical Densitometry and the International Osteoporosis Foundation, the DXA has become a go-to tool to measure BMD.

The era of ERAS! #SurgicalPearl:
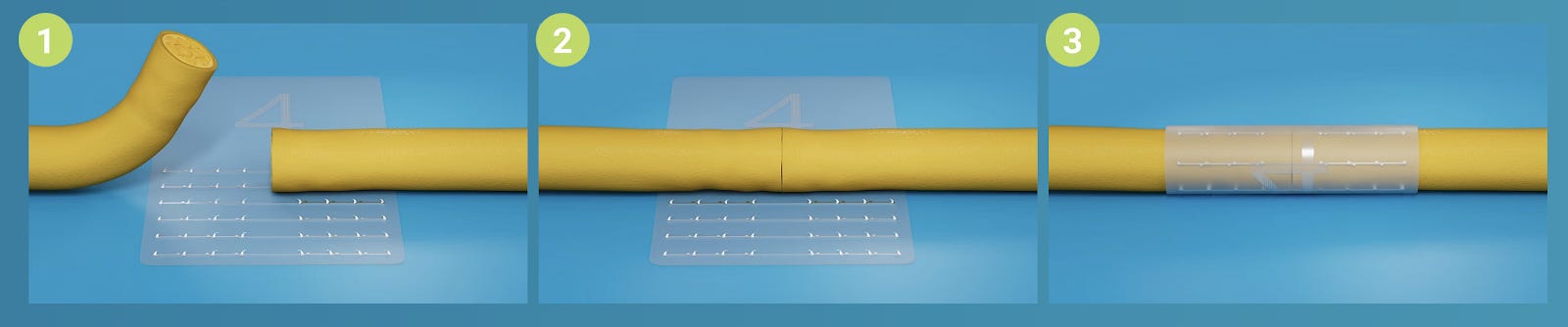
Erector spinal plane block is one of the best tools for “Enhanced Recovery After Surgery” (ERAS) approach enabling Same-Day Discharge Spine Surgeries
It targets the dorsal rami of nerve root and provides excellent pain relief post surgery.
Best part is it can be done under ultrasound or fluoroscopy guidance or just free-hand intra-operatively
-
Under GA, with the patient prone, a curvilinear US probe (2 to 5 MHz) is longitudinally placed over sacrum. The probe is moved cranially till the surgical level is identified. It is then shifted parasagittally, approximately 3 to 4 cm lateral to visualize the tip of the transverse process.
-
23G (90mm) spinal needle is inserted to contact TP using the out-of-plane technique (Figure).
-
Accuracy of the position of needle tip is confirmed using hydro-dissection with 1 ml of normal saline. The saline spreads evenly in the plane between the erector spinae musculature and TP without muscle distension.
-
Then local anesthetic like 20 ml of 0.25% bupivacaine is injected.
-
In an experienced hand, the whole process takes just 6 minutes. To know more read this RCT
IR Guided Biopsy is a true saviour #MostCited:
In kids, the diagnosis of osteomyelitis becomes challenging. The symptoms are vague. There are very little clinical clues. Blood cultures don’t give any hope. A surgeon is forced to convince parents to the lesser evil (surgery) to avoid the dealier chronic disease.
Interventional Radiology (IR)-guided percutaneous biopsy is the savior of surgeons in such situations. Gajewski et al. analyzed the utility of IR-guided biopsy compared to empirical treatment in 50 acute hematogenous pediatric osteomyelitis cases. Fifteen (30%) had IR-guided biopsies; 35 (70%) were treated empirically. Of the 15 patients who underwent IR-guided biopsy, a pathogen was identified in 12 cases (80 %); 14 of these patients had concomitant blood cultures with only 1 (7%) positive result (P<0.01). The average time from blood sample collection to definitive antibiotic initiation was nearly double that of time from IR-guided biopsy collection to definitive antibiotic initiation (70.8 vs. 36 h; P<0.01).
So IR-guided biopsy is something to adopt

Where to inject - rotator interval or posterior capsule? #InTrials:
Traditionally injecting steroids through the posterior capsule of shoulder has been common for frozen shoulder. Injecting through rotator interval (RI) is not prevalent for reasons like the technical difficulty involved. But, RI seems to be the area of pathology. Injecting through RI makes more sense. Cho et al have shown that injecting through RI leads to statistically significant better ROM than through posterior caspule though the accuracy of RI injection was low. The improvement in pain and functional outcomes remained the same between both groups in this study.
Injecting through RI might have its benefits!

Answer for last month questions:
What is the most effective route of selective nerve root block in spine?
-
Transforaminal
-
Interlaminar
-
Caudal
Events to check out:
-
2023 AOA Annual Scientific Meeting
12-16 Nov, 2023 - Melbourne, Australia
-
AO Sports Advanced Course - Knee Injuries and Deformities
10 - 13 December 2023 - Davos, Switzerland
-
January 26, 27 2024 - Pune, India
Question of the month:
Which modality is more sensitive and specific to diagnose rotator cuff tears?
-
MRI
-
MR arthrogram
-
USG
Sit tight till the start of November to know the answer
Have a marvelous month ahead guys. Cya!