Starwars Super Weapons, Scales' Story, Stonewalls and more
Enjoy the exclusive issue on Orthopedic Oncology
The Starwars Super Weapons are coming - #NeoArmory
Bone tumor management is not for the light-hearted. Even if we walk through every step of making a correct diagnosis, plotting an out and out plan, and providing multimodality treatment very carefully, the results may not be soul-satisfying many a time.
The main culprit is R E L A P S E.
Solution?
“Sustained residual concentration of chemotherapy drugs at the site, without having systemic complications or affecting bone regeneration”
Too much to ask for?
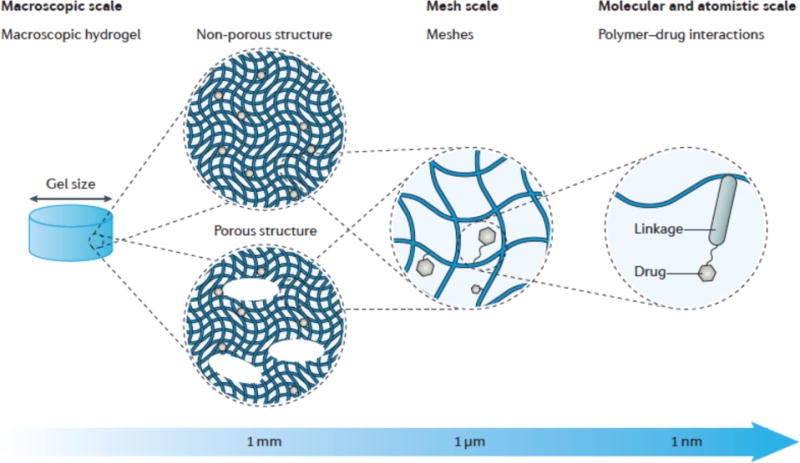
Well, there are drug-loaded Hydrogels.
These completely customizable biocompatible hydrophilic gel-based polymers can absorb drugs, and swell. They do not dissolve in a water-based environment. They can be programmed to release drugs continuously or in a pulsatile manner for short or long term
Though these wonderdrugs are still in the early stages of development, I can clearly see the light at the end of the tunnel. The Starwars Super Weapons are coming

From biomechanical to biomedical engineering - The Scales’ Story of evolution of expandable prosthesis
John Tracey Scales, a professor of biomechanical engineering managed to convince H J Seddon, the then director of the Institute of Orthopaedics, University of London, of the need to develop biologically inert plastics and developed a knee prosthesis made of stainless steel and acrylic polymer which was successfully used, the first operation of its kind in the world. Scales went on to develop the first Stanmore total hip replacement and replacements for the elbow, and shoulder in collaboration with eminent orthopedicians. In 1974, Scales established the department of biomedical engineering, the first such university department in Britain.
Prof Scales' greatest contribution was along with Rodney Saville Sneath in the development and use of extendable prostheses for children, the first of which was inserted in 1976.
He also developed porous wound dressings and created a low air loss mattress for use in the treatment of severe burns and severe pressure sores. This work led to his appointment as honorary director of research at the RAFT Institute for Plastic Surgery at Mount Vernon Hospital, Northwood. Scales contributed 175 articles to professional journals and books. The UCL Scales’ prize is awarded every year to honor him.

A Capanna modification from Lu et al - #SurgicalPearl:
For large bone defects after tumor excision, Lu et al have proposed a modified Capanna technique using frozen tumor-bearing autograft and vascularised fibular graft.
The essential steps are
-
Osteotomy must be performed at least 1 cm from the margin of the lesion identified in MRI images and fast-frozen pathology
-
Specimen separated from the surgical field was prepared and slotted laterally to facilitate implantation of the fibula flap,
-
The bone segment was irrigated sequentially with 3.0% hydrogen peroxide, then physiological saline, followed by freezing in liquid nitrogen for 35 minutes.
-
Vascular Fibular Graft was harvested using a standard lateral approach. The length of the fibula was 3 cm to 4 cm longer than the bone defect,
-
VFG was passed through the central cavity of the frozen autograft, assembled at the defect site, and plated.
Do check out their paper here
Are our stonewalls strong enough? #MostCited
Are our routine aseptic steps and antibiotic prophylaxis strong enough to counter infection in endoprosthetic replacements?
The Delphi study in the 2018 international consensus meeting on musculoskeletal infection concluded that there is no need to prolong the routine antibiotic prophylaxis following endoprosthetic replacement surgery; There is no need to change antibiotic prophylaxis based on chemoradiation status; No evidence to soak endoprosthesis in antibiotic solution prior to implantation; Drain if used can be removed within 24 hrs of surgery, And PJI involving endoprosthetic replacement and routine total joint replacements can be treated the same way.
Seems like our stonewalls are strong enough!

What do the ratios tell us?
A successful sarcoma surgery does not mean a good prognosis. Seo et al. retrospectively analyzed the Orthopaedic Oncology Database to find the preoperative parameters to prognosticate the survival of sarcoma patients. Inflammation plays a major role in tumor development, progression and metastasis. A high preoperative lymphocyte-monocyte ratio is significantly associated with better overall survival and prognosis in sarcoma patients. In contrast, a high preoperative neutrophil-lymphocyte ratio is significantly associated with shorter overall survival and poorer prognosis.
What do the ratios tell us? - #Prognosis

Check out these cool events:
-
3rd International Conference on Orthopedics Dubai, United Arab Emirates
-
2nd International Conference on Arthroplasty and Orthopedic Surgery – Hybrid Event Paris, France
-
IOACON 2022 Amritsar, India.
Answer to the July question:
Can the fixation of periprosthetic fractures of the hip and knee be delayed >24 hours?
Answer: No
Delay in fixation increased the 30-day mortality rate according to a meta-analysis involving 3006 patients
Question of the month
Which adjuvant therapy has a better depth of necrosis in the treatment of benign bone tumors?
-
Phenol
-
PMMA
-
Argon Beam Coagulation
-
Liquid nitrogen
Wait for our September issue for the answer????
Have a fabulous month ahead folks. Love y’all tons!????????