Time for a HIP-Hop
Enjoy reading on hip; hope you enjoy hip-hop in the background as well!

Straight from the MARVEL comics
One of the difficult to conquer territories in Trauma management is fragility fractures of the hip. Fragile patients combined with porotic bones; prime directive becomes avoiding failure rates. Implant cut-out is one of the main henchmen of failure.
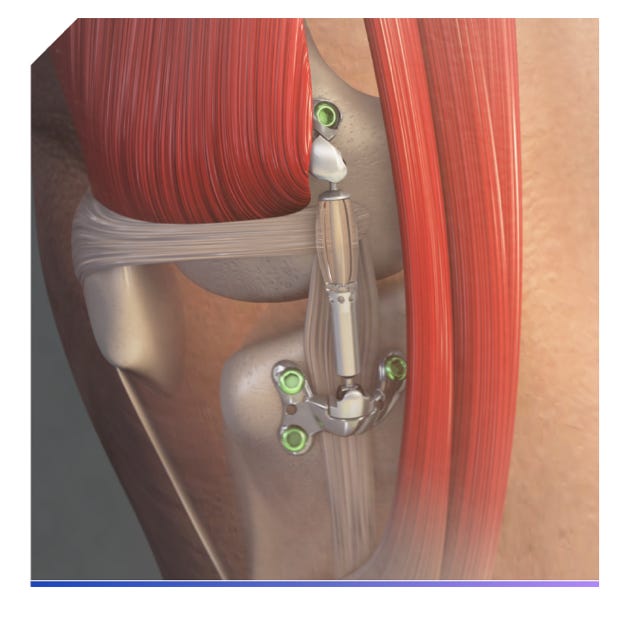
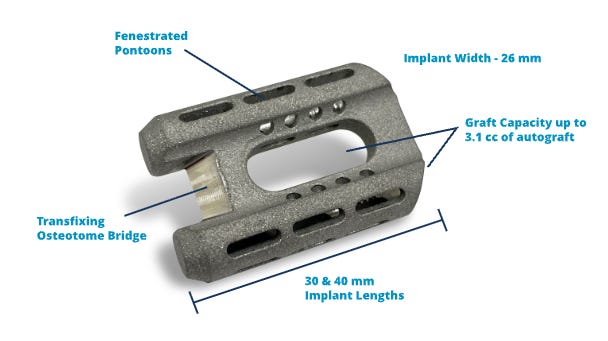
We have tried many ways to overcome this, of which the recent methods being cement infusion. But today’s implant is straight from the marvel comics, especially feels like it’s been made by Tony Stark himself. Introducing “X-Bolt”, a screw with a deployable expansion unit that causes compaction of the bone around and provides rotational stability. This is available currently as XHS (X-bolt hip [plating] System) or as X-Bolt Pro-X1 trochanteric nail system.
Biomechanical studies show this has 25% greater peak load, 425% greater peak torque, requires 24% greater peak force to cut out, better torsional stability, and a superior cut-out resistance at various Tip-apex distances than a DHS. ‘WHiTE4’ trial, a blinded RCT showed no statistical difference in HRQoL (Health-Related Quality of Life) at 12 months.
If the biomechanical characteristics can mirror the in vivo performances, then the X-Bolt is here to stay.

Bern gave it all!
Be it Replacement, Preservation, or Fixation!
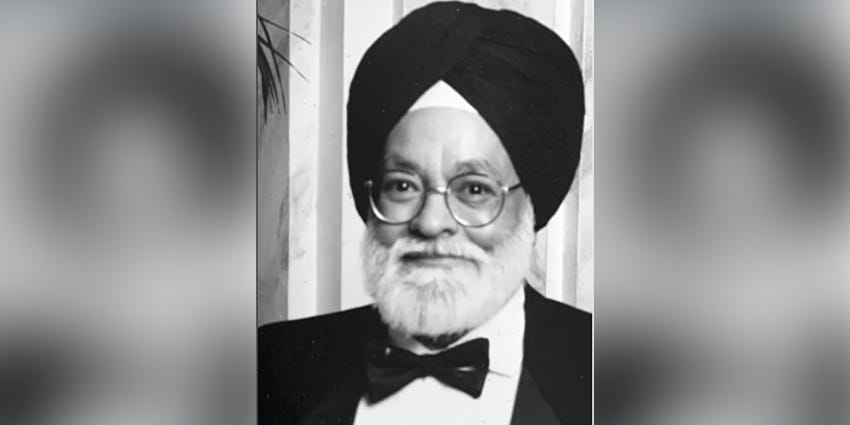
The Inselspital, or University Hospital of Bern, Switzerland holds a prominent place in the development of modern-day hip surgeries. It is the place of Emil Theodor Kocher, a Nobel prize laureate with important contributions in Orthopaedics and Surgery.
From 1963 to 1980, Prof. Maurice Edmond Muller chaired the Dept. of Orthopaedics at Bern. In the 1960s Muller was instrumental in developing Hip replacement prosthesis inspired by Sir John Charnley. He founded AO which went on to revolutionize internal fixation in Orthopaedics. He was also a founding member of the International Hip Society. SICOT aptly named Muller as the “Orthopaedic Surgeon of the Century”

The baton was then passed to Prof Reinhold Ganz who headed Orthopaedics at Bern from 1981 to 2004. He has influenced a whole generation of orthopedic surgeons through his research, surgical innovations, and teaching. He investigated hip dysplasia, performed pioneering research into the vascular supply of the femoral head, and devised the Bernese Periacetabular Ostectomy – that allowed correction of the acetabular deficiencies with accuracy, predictability, and acceptable morbidity. He also recognized femoroacetabular impingement as a cause of osteoarthritis. He gave the world “Safe surgical dislocation” and devised surgical strategies to treat the pre arthritic hip. His systemic pursuit of an understanding of these conditions established him as the leader of conservative hip surgeries
Professor Ganz authored nearly 460 publications. In addition to the King Faisal International Prize for Medicine, his contributions were recognized by many other awards, including the Prix Mondial Nessim HABIF de Chirurgie of the University of Geneva and the Arthur Steinder Award of the Orthopedic Research Society, among others.
Prof. Klaus A. Siebenrock helms Orthopaedics in Bern since 2005. Together with his team, he is furthering hip joint preservation surgeries to the highest level.
Do attend the Bern Hip Symposiums!
Technical Pearl - Correct cup inclination with spirit level!
Robotics is the latest to position components accurately in THA on one side of the spectrum; On the other side though Khalifa et al have adopted yet another tool from the architecture field to aid in accurate cup positioning.
Results of using Spirit level mobile freeware seems accurate to 3 degrees in their study
The methodology is quite simple.
The table is made parallel to the floor using the app. The pelvic tilt is measured after positioning as an angle between lines connecting both ASIS and floor. The phone with the app installed is sealed in a sterile cover. An ex-fix rod clamped to a supra-acetabular Schanz pin at an exact angle of 40 degrees (of course using the app) is used to direct the reamer for acetabular reaming. This is done after neutralizing the pelvic tilt.

Well! We are known for brevity. Check it out yourself.
PelviXNet: The Next-Gen Pelvis Radiologist!
Radiographs of the pelvis remain a vital component of the trauma survey. Their interpretation is getting a fool-proof system soon.
Cheng et al. developed a multiscale deep learning algorithm called PelviXNet trained with 5204 pelvic radiographs with weakly supervised point annotation. PelviXNet yields an area under the receiver operating characteristic curve of 0.973 (95% CI 0.960-0.983) and an area under the precision-recall curve of 0.963 (95% CI 0.948-0.974) in the clinical population test set of 1888 pelvic radiographs. The system is 92% accurate with 91% sensitivity and 93% specificity and demonstrates comparable performance with radiologists and orthopaedicians in detecting pelvic and hip fractures.

α-2 PIC: A Novel Biomarker of VTE
Trauma patients, particularly pelvic fractures, have an inherent risk of venous thromboembolism, and universal administration of VTE prophylaxis has its own limitations.
α-2 PIC is alpha 2-plasmin Inhibitor-Plasmin Complex identified by Guo et al. as a biomarker for VTE by assessing plasma levels of α-2 PIC and VTE risk using Caprini risk assessment score in 683 trauma patients. Patients with VTE had significantly higher levels of α-2 PIC than those without, after adjusting for confounding factors. Also, α-2 PIC increased in a stepwise fashion with increasing VTE risk.

Check these cool events that line up:
-
7th EPOS BAT INSTRUCTIONAL COURSE TRILOGY (Part I) for Pediatric Orthopods out there
-
21st European Congress of Trauma and Emergency Surgery - Norway this time
-
Face Ahead from AO to inspire the next generation
The answer to the last issue Query is here
How long do you think a hip replacement would last?
25 years in around 58% of patients receiving THR.
(Based on a systematic review and meta-analysis by Evans et al. from a 25-year pooled survival of hip replacements from forty-four case series including 13 212 total hip placements and from joint replacement registries with ninety-two series including 215 676 total hip replacements)
Question of the Month
Which method of ankle fusion do you think is the better way of doing it?
Open? Or Arthroscopic?
Evidence-based answer mind you!
Wait for the March-ing Foot & Ankle Special issue????
Have a fabulous February!