Dealing with complications of life
PS: this is not about better-halves
The USB adapter of Hip revisions
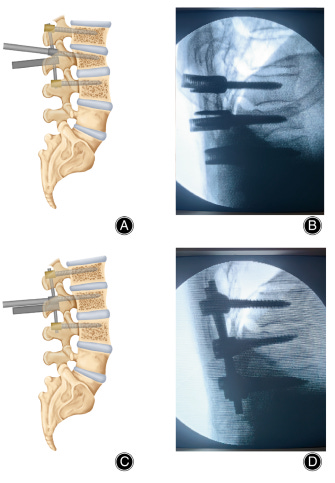
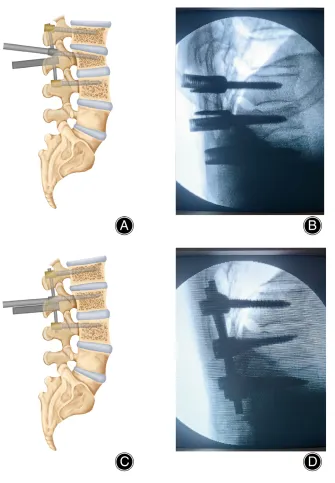
What’s the first rule of Orthopaedics? It is “Thou shall not Varus”. The Second rule? It’s “Thou shall not mismatch tapers” (Yep, we read the commandments). With Globalisation and medical tourism picking up pace, we’re already revising Total Hips from another generation or manufacturer who has become obsolete or even from another continent.
And it is not uncommon to find well-fixed stems only to be taken down because the tapers didn’t match. What if, we had a USB-adapter-converter-sorts to help with the problem?

That’s where the Merete BioBall® System comes in. Their taper adapter sits on top of the stem while in addition to allowing taper conversion, also allows adjustment of offset, neck length and best of all the version (to an extent).

They also have customizable adapters and a patented adapter selector.

Offset Adapter
A taper mismatch can raise the failure rate and Metere provides a simple and elegant solution. The primary indication is isolated acetabular revision. Studies show complication rates around 7% with a re-dislocation rate between 5.2-15%.
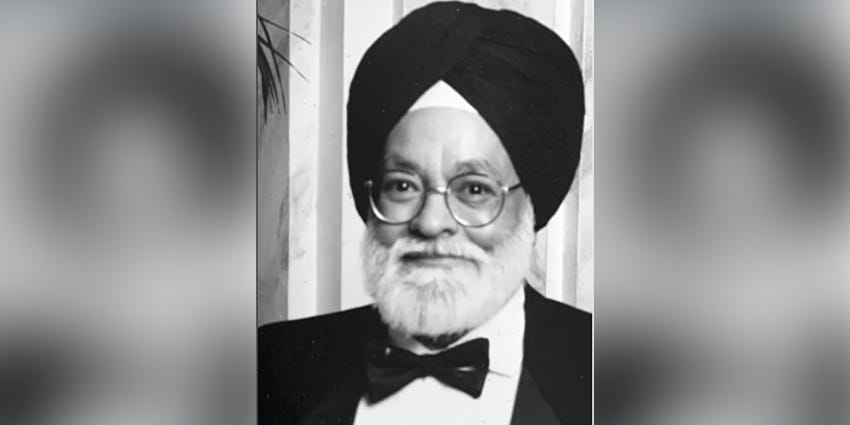
The Evolution of Osteotomy: #FromTheHistory:
The idea of fixing bone alignment goes back, like way back to 1600 BC found written on Edwin Smith Papyrus. Even Hippocrates in the 4th century BC was into correcting the deformities and he used his self-made contraption called Scamnum. Almost for 12 centuries nothing much changed but in the 16th century they started breaking the bones and re-setting them and they called it Osteoclasia, like a prequel to Osteotomy. They even used book presses to straighten the deformities and all this without anaesthesia and X-rays, imagine that!
By the late 18th century, the scene became more invasive with the introduction of saws, drills, gimlets, and carpentry chisels to perform what they called Subcutaneous Osteotomy. But without germ theory and sterility, consequences were gruesome with infections and some of them ascribed it to foreign body reaction to sawdust from bones! Not until William MacEwen published his first case series in 1879 and his exclusive book on Osteotomies, did his observations in around 1800 patients without major complications - Thanks to germ theory and sterility which were which were taking baby steps at that time.
Now, taking this idea of correcting the deformities and translating it to deformities secondary to osteoarthritis took around 6 decades, when Wardle presented his 35 cases for whom he did High tibial osteotomy (HTO), same procedure which was being used by Sir Robert Jones for childhood rickets since 1928. Mind you, they were not fixing the osteotomies. They were only immobilising till Coventry from Mayo Clinic USA started using staples, and Werner Mueller from Switzerland started using AO T-Plate to stabilize the osteotomy. Even today, we are seeing an evolution of implants towards a better fixation and early mobilisation but it’s a joy to find out how we reached where we are today.
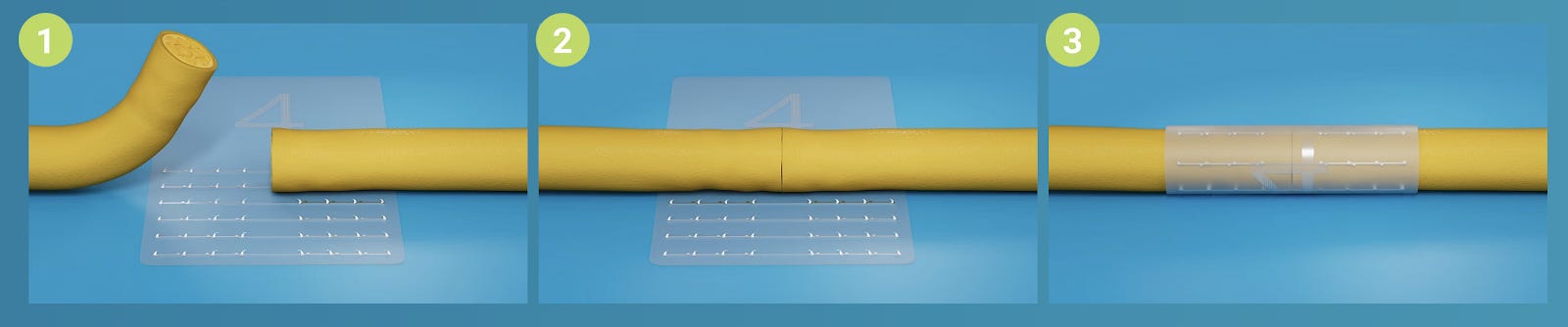
Glove before Gown or Gown before glove - #TechnicalPearl:
Many of us don the surgical gowns while the scrub staff helps us wear the gloves in a sterile manner. This can be a closed technique where only the fingertips are outside or an open technique where the fingers are outside before wearing the glove.
Some of us wear the gloves first. Which is the right way to avoid infections?
Well, the Glove-first technique seems to be ideal.
-
Don the under gloves first,
-
Don the gown,
-
Wear the outer surgical gloves
This might seem like a minor modification of our practice. However, this technique had zero contamination when compared to open and closed staff-assisted techniques according to Byrd et al. This might help us avoid surgical site infection!.

It says ASPIRIN - #FightAgainstVTE - #InTrials:
Conducted by the Major Extremity Trauma Research Consortium (METRC), a multicenter trial involved over 12,000 patients aged 18 and older who had undergone operative treatment for fractures or suffered pelvic or acetabular fractures. Patients were randomly assigned to receive either aspirin or heparin for Venous Thrombo-Embolism (VTE) prophylaxis
The results were against the wave - Yes, aspirin was non-inferior to heparin in preventing death from any cause at 90 days, with similarly low incidences of pulmonary embolism and bleeding complications. Though the incidence of deep-vein thrombosis was slightly higher in the aspirin group, the overall findings suggest that aspirin may offer a comparable alternative to heparin for thromboprophylaxis in fracture patients. Aspirin seems to be a safer and more accessible option for preventing thrombotic events in this patient population.

Aren’t the results ready yet? How many days should I wait?
Right now culture remains the gold standard diagnostic test to diagnose PJI. But how long should one wait to know the results on positivity and is the routine 3-day culture sufficient? Tarabichi et al. came out with these results from their multicentric study after analysing the results of 536 positive cultures. Let’s know the waiting time to effectively identify the common culprits.
-
Gram-negative organisms - 1.99 [1.1 to 4.1] days
-
MRSA - 1.42 [1.0 to 2.8] days
-
MSSA - 1.95 [1.1 to 3.3] days
-
Streptococcus species - 2.92 [1.2 to 4.3] days
-
Staphylococcus epidermidis - 4.20 [2.4 to 5.5] days
-
Candida species - 5.30 [3.1 to 10] days
-
Cutibacterium acnes - 6.97 [5.9 to 8.2] days
As per the sample to be sent for identifying them synovial fluid showed the fastest positivity at 1.97 days followed by soft tissue and bone at 3.17 and 4.16 days respectively.
Events to check out:
-
68th Annual Congress of the Korean Orthopaedic Association 17-19 October 2024 -Seoul, South Korea
-
DKOU 2024 - German Orthopaedic Congress - 22 - 25 October 2024 - Berlin, Germany
-
12th Emirates International Orthopaedic Congress 15 - 17 November 2024 - Abu Dhabi, UAE
Answer to last month’s question:
What percentage of SCFE cases could have thyroid involvement in their pathogenesis?
-
<10
-
10-20
-
20-30
-
>30
According to Nielsen et al. more than 30 percentage of children with SCFE had an associated hypothyroid state and affected the treatment of SCFE in 24% of cases. Thyroid screening should be included as a part of routine workup in SCFE.
Question of the month:
What is the rate of deep infection in case of aseptic revision fracture fixations?
-
5%
-
10%
-
15%
-
20%
Watch out for this space next month to know the answer.
Have a Joyous July guys