In war against cancer
Enjoy reading the exclusive issue to get better equipped in the war against cancer #OrthopaedicOncology
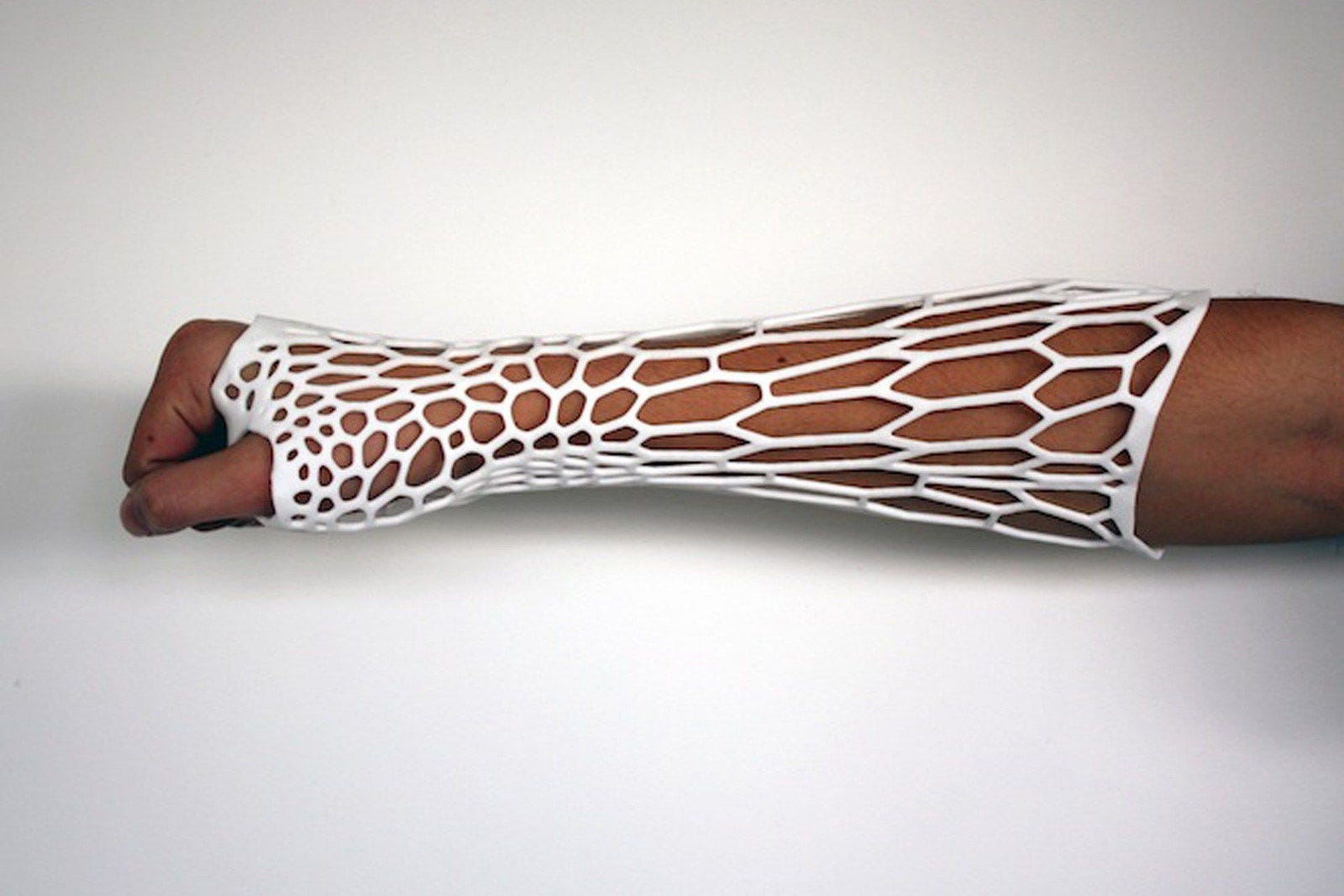
Perfecting endoprosthesis - #NeoArmory:
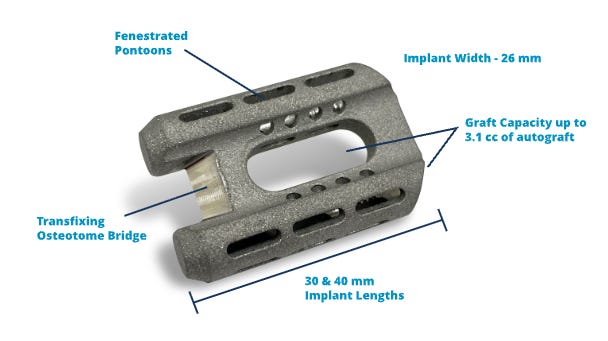
Okay, who said Orthos don’t care about soft tissues? Case in point, our Implant for this month – ELEOS, the Proximal tibial Limb salvage system from Onkos surgical.
The New Jersey-based company with an impressive bone tumor portfolio has designed a proximal tibia reconstruction prosthesis that allows soft tissue ingrowth. Soft tissue failure is noted to be one of the 5 major reasons for Tumour Endoprosthesis failure. The implant is designed with a Pore size range of 502-758μm which is supposed to promote soft tissue integration.

In addition to this, the bone-implant interface is Modular Bio GripTM which is HA coated; a 3D-printed collar improves osseointegration. This is a nano HA coating that aims to be smaller and superior. The implant seems promising. Do follow us to know about the clinical outcomes of using this implant.

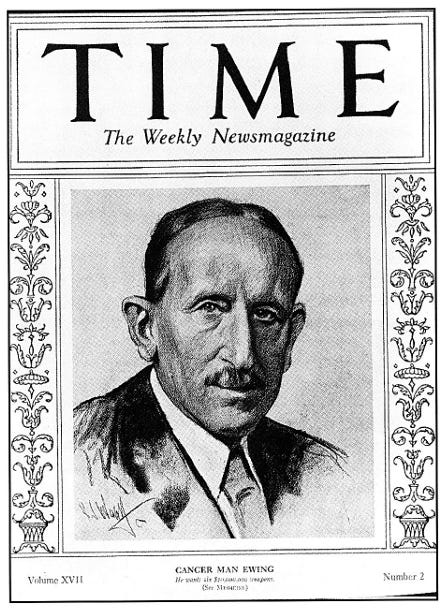
The Cancer Man: #FromTheHistory:
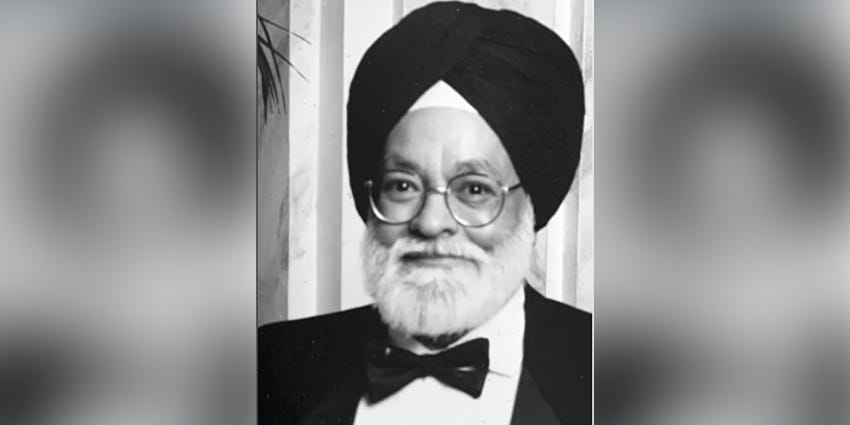
It is really unfortunate but not uncommon to come across men who lived and died fighting cancer. It is, however ironical and rare to find someone who lived his whole life helping people fight cancer and died of cancer.
The magnanimity of his contributions to cancer research can be understood by the fact that Time Magazine named him “The Cancer Man”. He was fondly called Mr. Cancer. Though he was honored with an eponymous tumor - Ewing’s sarcoma, the honor is an understatement for his works.
James Ewing had a painful childhood with tibial osteomyelitis. He was a widower and suffered trigeminal neuralgia and hip ankylosis. The mental and physical pain that he suffered made him more compassionate towards cancer patients which he channelized into research. He made significant contributions to the understanding of infectious lymphosarcoma in dogs. He co-founded the American Association of cancer research. He was instrumental in setting up Memorial Hospital (now - Memorial Sloan Kettering Cancer Center) as an exclusive cancer center. He worked on the uses of radium in cancer treatment and was one of the very first to use radiotherapy for cancer treatment. In 1920, he presented his findings on a new form of bone tumor from the diaphysis which is radiosensitive. He named it endothelioma of bone which later was named Ewing’s sarcoma to honor him. It was unfortunate for him to succumb to bladder cancer in his later years.
Denosumab k(NO)w need - in GCTs: #InTrials:
A Randomized phase III trial evaluated the usefulness of denosumab before curettage for giant cell tumors of bone. The trial included a total of 18 patients, Eleven patients were assigned to Arm A (curettage and adjuvant local therapy) and 7 to Arm B (preoperative denosumab, curettage, and adjuvant local therapy). Relapse-free survival proportions in both arms were 90.0% and 100% at 1 year, and 60.0 and 62.5% at 2 years. The study concluded in terms of relapse-free survival, the superiority of preoperative denosumab was not observed in patients with giant cell tumors of bone without possible post-operative large bone defect.

Save the (proximal) femur - #Surgical Pearl:
Salvage has become the word to look for in Onco world. Xu et al have come up with a new technique for saving proximal femurs - “The Pedicle frozen allograft-prosthesis composite reconstructions for malignant bone tumors involving proximal femur”
Ideal candidates: Patients with osteoblastic neoplasms or tumors causing destruction of less than one-third of cortical bone. What if patients have greater bony destruction? Bone defect needs to be augmented with bone cement or graft
-
Lateral approach and wide excision with adequate surgical margins of the surgical biopsy tracts and extraskeletal mass.
-
The joint is then dislocated and the gluteus medius is peeled off the greater trochanter, maintaining the continuity with the fascia lata
-
The bone marrow and tumor are then removed from the medullary cavity. The surrounding normal soft tissues are then protected by surgical sheets before immersing the proximal femur in liquid nitrogen.
-
All the muscles and tendons are detached from the proximal femur until the femur can be completely rotated and immersed in liquid nitrogen
-
An additional 2 cm bone away from the margin of the bony lesion is then inserted in liquid nitrogen by pedicle freezing method for 20 minutes, followed by thawing for 15 minutes at room temperature; and in distilled water for 15 minutes
-
Following this, an intertrochanteric osteotomy is performed (preserving the greater trochanter); and cemented, long-stemmed bipolar hemiarthroplasty is performed. The gluteus medius musculature is then reattached to the original anatomical site using braided, polyblend, polyethylene bone-to-tendon sutures
NB: A tourniquet is utilized to prevent bleeding and tumor dissemination during the pedicle freezing. Check out the full technique here.


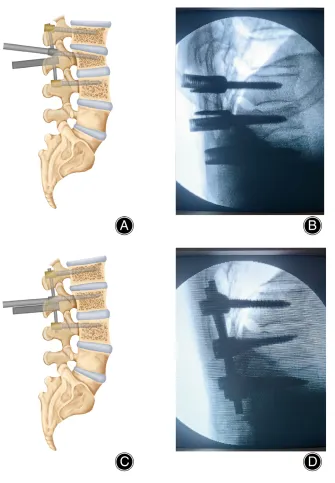
Cometh the radiolucent nails! - #HighlyCited
How many of you wanted to invent a radiolucent nail just to spare the headache of screening for recurrence through distorted metallic artifacts after prophylactic nailing in onco patients?
Well, carbon fiber nails are coming!
Yeung et al. compared the results of 72 patients who underwent prophylactic or therapeutic fixation for pathological long-bone fractures with titanium or carbon fiber nails.
Patients receiving carbon nails had higher blood loss (median 150 ml vs 100 ml; p = 0.042) and longer fluoroscopic time (median 150 seconds vs 94 seconds; p = 0.001). But, Implant complications occurred in seven patients (19%) in the titanium group versus one patient (3%) in the carbon fiber group (p = 0.055). Also, there were no notable differences between groups with regard to surgical wound infection, or survival.
Carbon nails seem promising! Watch out this space for more updates.
Events to check out:
-
North American Spine Society (NASS): NASS Annual Meeting Los Angeles, USA: 18-21 October 2023
-
National Congress of the Italian Society of External Fixation (SIFE), Milan, Italy 27-28 October 2023
-
43rd SICOT Orthopaedic World Congress 21-23 November 2023
Answer for the last month question:
Can we use Aspirin for thromboprophylaxis following fracture?
Answer: Yes
In patients with extremity fractures that had been treated operatively or with any pelvic or acetabular fracture, thromboprophylaxis with aspirin was non-inferior to low-molecular-weight heparin in preventing death and was associated with low incidences of deep-vein thrombosis and pulmonary embolism and low incidences of deep-vein thrombosis and pulmonary embolism and low 90-day mortality. Check out this trial published in NEJM recently
Question of the month:
Pathological Fracture in Osteosarcoma - which of the following is false?
-
Contraindication for limb salvage surgery
-
Associated with the increased rate of metastasis
-
No difference in recurrence rate when compared to those without pathological fracture
-
Decreased 3-year and 5-year survival rate
Hold your curiosity till our next issue.
Have a great month ahead.