Saviour of sick kids
Enjoy your brew reading this special issue on paediatric orthopaedics
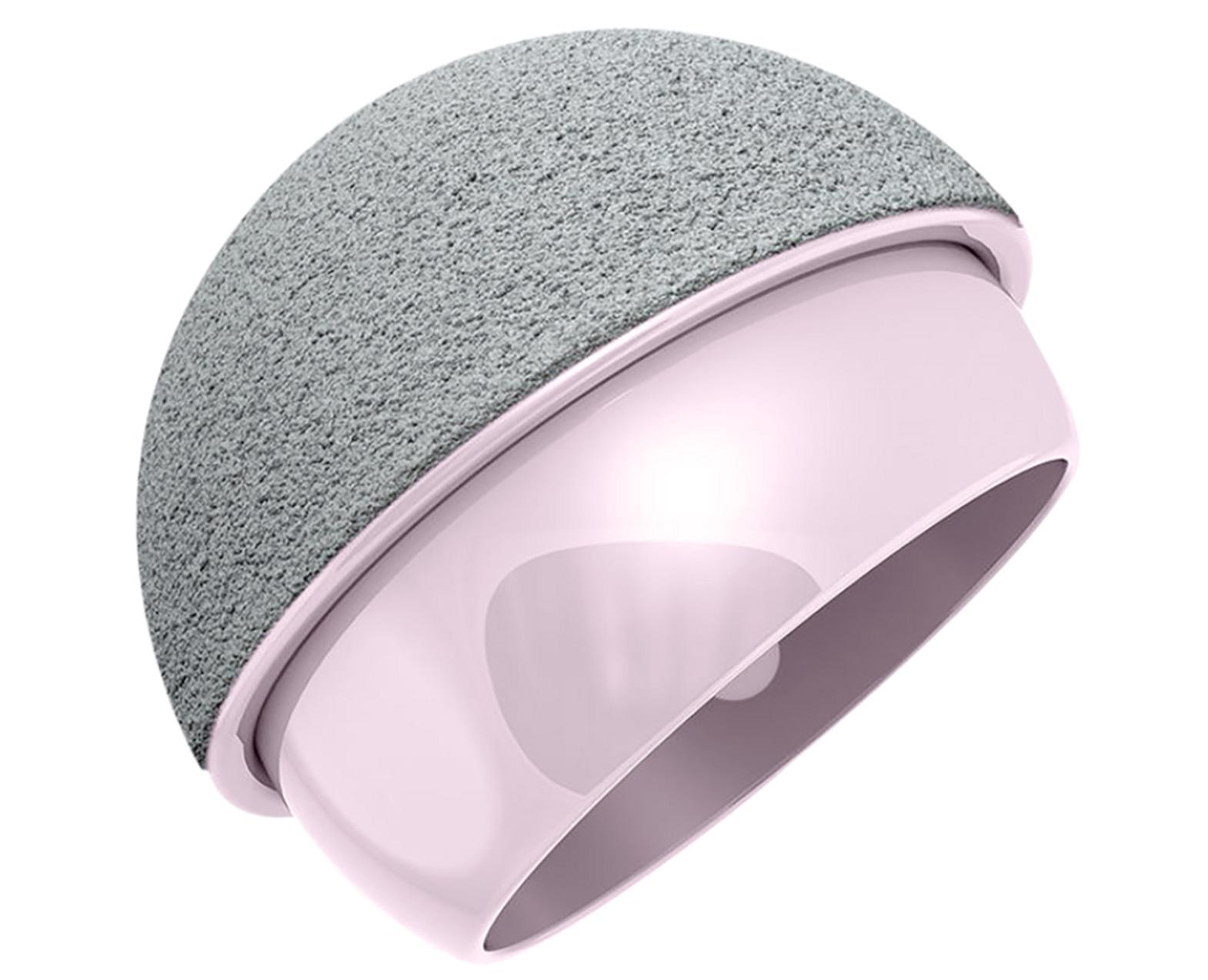
No more implant exits!
Circa 2000:
Me: Your kid sustained a displaced distal tibial epiphyseal injury
Kid’s parent: (after breakdown and consolation) What has to be done doc?
Me: It needs fixation probably with metal screws.
Kid’s parent: metal? you are going to remove it back right? ain’t there any resorbable screws?
Me: We can remove them, but after a year… resorbable screws with good strength are a distant dream as of now
Circa 2015:
……
Me: We can remove them, but after a year… resorbable screws with good strength are still in the research phase
2023:
….
Me: There are some FDA-approved screws! (Can you guys see the hope on parent’s face?)
Yes, guys.. bioresorbable metal screws have come a long way from research to reality. FDA for the first time approved a bioresorbable metal screw - RemeOS screw for trauma in 2023. The RemeOs screws by Bioretec represent a groundbreaking advancement in pediatric orthopaedic implants. Composed of an alloy of magnesium, calcium, and zinc—the RemeOs screws provide the necessary strength, rigidity, and hardness for heavy load-bearing, such as those required in foot and ankle surgeries. RemeOs screws gradually dissolve and are replaced by new bone tissue as the injury heals. The innovative composition and design of RemeOs screws offer superior mechanical properties compared to polymer-based bioresorbable implants, making them ideal for a variety of applications in orthopaedic trauma.

The product is new with some whitepaper reports on the company website and a few published case series. So be cautious if you are trying out guys.
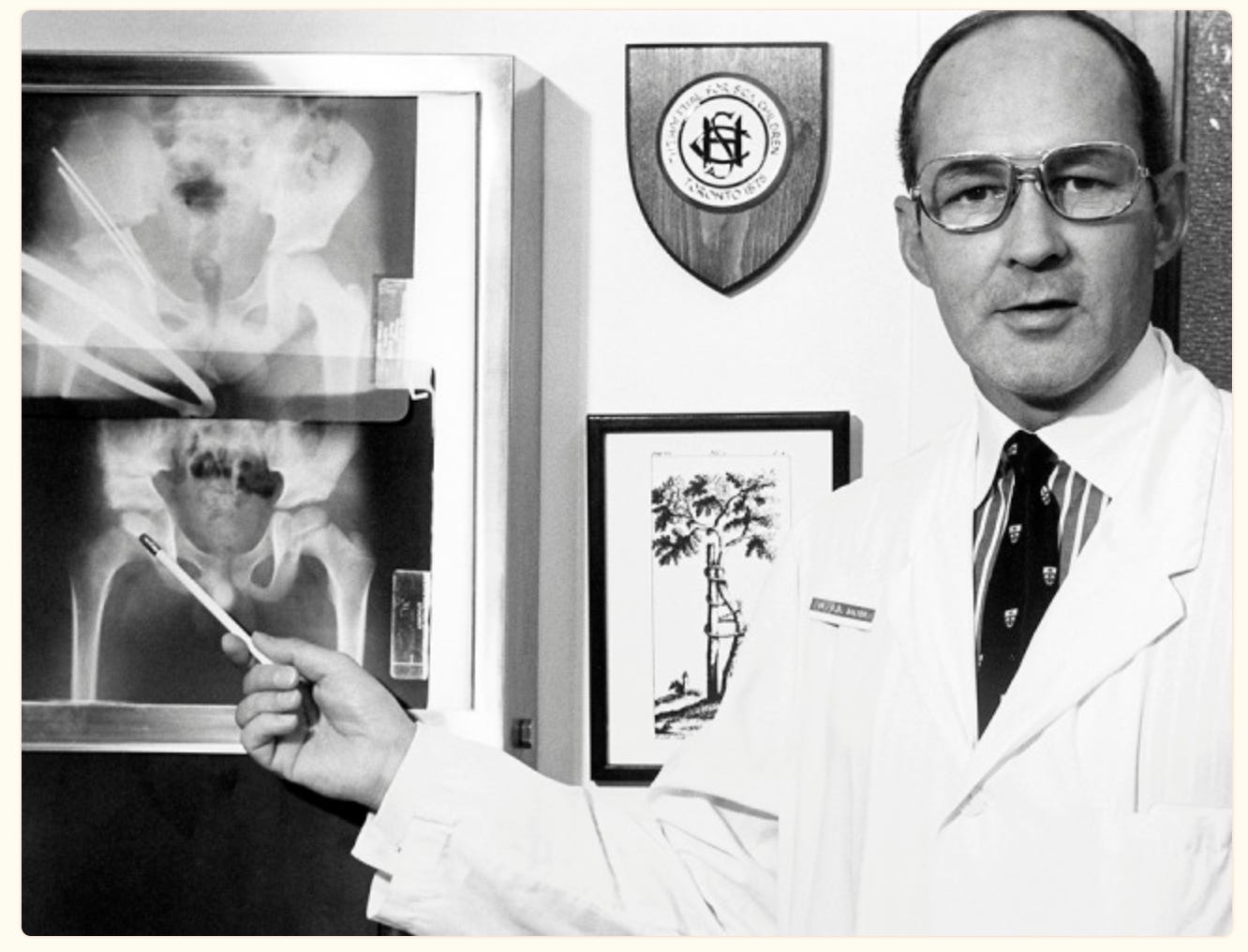
Importance of passivity: #FromTheHistory:
After completing his residency in Canada, a young lad moved to Britain to get trained under legends like Sir Reginald Watson-Jones at the London Hospital. The dictum of Watson-Jones was rigid prolonged immobilisation of fractures. But the intuition of Robert Salter felt otherwise. He felt that the dogma must be false at least in joints. In the most academic way of revolting, he began a series of experiments with continuous passive mobilisation of joints. His experiments led to the development of the concept of Continuous Passive Mobilisation of joints.
His inquisitive mind also led to the development of innominate osteotomy aka Salter osteotomy for developmental dysplasia of the hip which he would refer to with a pun as no name - no fame osteotomy. Before the introduction of this osteotomy, DDH was considered a grave disease with devastating complications. He also contributed to the development of the classification of epiphyseal injuries - the Salter and Harris classification.
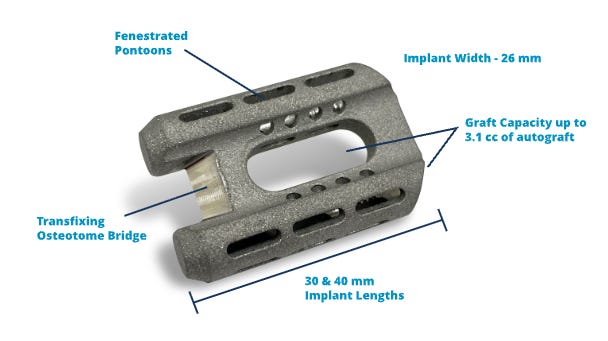
Guided growth - ?a breakthrough in the management of CPT #SurgicalPearl
Congenital pseudoarthrosis (CPT) of the tibia is a headache to any paediatric orthopaedician. Given the high failure rate of different surgical techniques, preventing CPT, if that is possible, would be great.
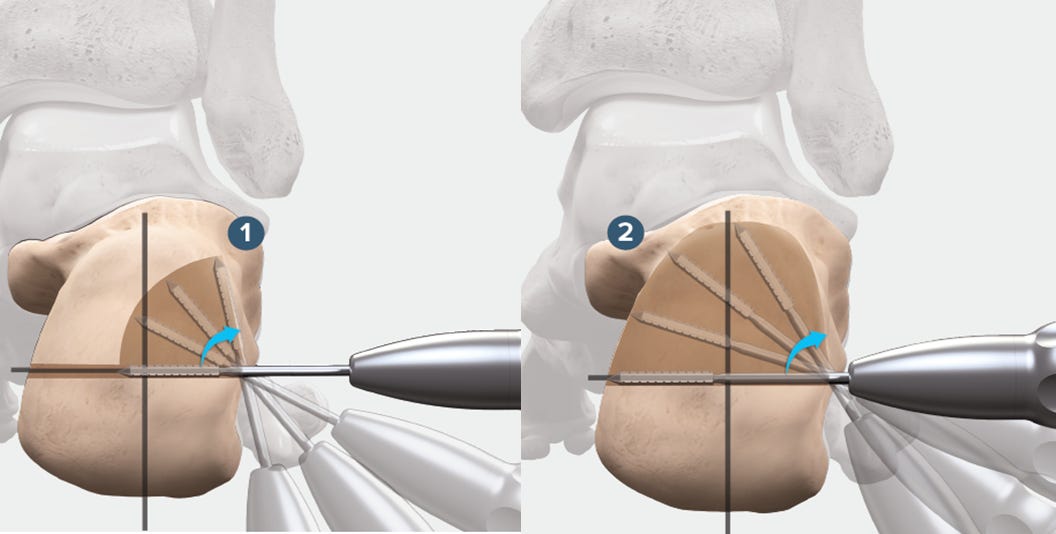
Well, that might well be possible, with encouraging results by Kennedy et al and Laine et al. Their technique of applying of guided growth plate to the distal tibia in cases with anterolateral tibial bowing has corrected the alignment and prevented the pseudoarthrosis development.
-
The point of maximal tibial bowing in an oblique plane was identified
-
A 1 to 2-cm incision was made over the distal tibial physis anterolaterally, in line with the plane of maximal deformity.
-
8 plate was applied across the epiphysis in a standard manner.
-
Patients were put on AFO braces till skeletal maturity.
-
Plate exchange was done when screws became too divergent. Plates were removed when the proximal and distal tibial epiphysis became parallel, and the alignment improved

Burning the midnight oil! - does it matter in supracondylar humerus fractures? #MostCited:
Supracondylar Humerus (SCH) surgical management < 18 hours is now considered a quality metric to rank hospitals in the US and many other countries. Many times the senior pediatric ortho guys should do back-to-back night calls to operate these trauma cases as and when they arrive. Does it make any difference in patient outcomes? Sullivan et al. in their study analysed the outcomes of surgical management in 435 patients who received surgical treatment within 18 hours and 37 patients who received surgical treatment >18 hours for SCH fracture.
Fractures in the ≥18-hour cohort were treated more commonly with 2 pins (62.2% vs. 38.5%, p=0.04). There were no statistically significant differences in open versus closed reduction, utilization of medial pins, or postoperative immobilization between cohorts. No differences were noted in postoperative complications, including non-union, delayed union, stiffness, malunion, loss of reduction, iatrogenic nerve injury, or infection. Though it may seem pressing, the <18-hours to surgery rule for SCH management does not seem to influence patient outcomes after all.
POCUS vs Xray: #InTrials
Is radiation from X-rays hazardous? This is the most frequent question of Google-educated young mothers who bring in their kids after a fall. Though we authoritatively explain that the dose of radiation after an xray is too minimal to worry, what if there is another modality which is more handy and accurate?
Point of Care Ultrasound (POCUS) might be that thing! Snelling et al in a multicenter, open-label, diagnostic RCT compared the accuracy of POCUS vs traditional x-rays in diagnosing paediatric forearm fractures. The trial enrolled 270 participants, and the results revealed that POCUS led to a significantly higher rate of correct diagnoses compared to radiographic imaging. 97.8% of participants in the ultrasound group were accurately diagnosed, compared to 83.0% in the radiograph group. POCUS was superior in identifying both "buckle" fractures and "other" fractures, without clinically important fractures being missed particularly in non-deformed forearms.
POCUS might be the future focus!

Answer to last month's question:

“Proximal scaphoid fx needs surgery” is the correct choice. Thumb immobilisation is not mandatory according to recent studies.
Events to check out:
-
British Orthopaedic Association Annual Congress 2024
17-20 September 2024, Birmingham, UK.
-
2 - 4 October 2024, Vienna, Austria
-
2024 Australian Orthopaedic Association Annual Scientific Meeting
13 - 17 October 2024, Brisbane, Australia
Question of the Month:
What percentage of SCFE cases could have thyroid involvement in their pathogenesis?