Steel spine and silver tongue
to have a silver tongue in Spine surgeries, read this special issue on Spine
Non-ionizing Navigation
Position – prep – scan – reference – (accidentally move reference) – huge sigh – re-reference – operate.

(Laughs in Robotic Arthroplasty)
Time to get one over our Arthroplasty colleagues! 7D Surgical is the world’s first company to use Machine vision technology for spine surgical procedures.

Machine vision?? Does anyone get it?
It uses their proprietary tech that consists of a camera which can directly recognize anatomy. This camera is embedded into the theatre lights. The patient’s CT is pre-fed into the system and the surgeon pre-plans the levels to be operated. Referencing is made intra-op and it takes 17 seconds to reference a level and about 30 seconds for a 2-level procedure, all done under direct vision of the camera.

Machine vision camera

It also gives you the trajectory of the instrument
If the reference point moves, the re-referencing seems a quick process as aptly marketed as ‘Flash-fix’. Evidence suggests this can reduce operating time by 63.6 minutes and reduce intra-op radiation exposure by 66%. Another study suggests 62% lesser blood loss (estimated) and 21% lower length of stay. Experiences suggest it takes about 9 cases to get used to it.

Spine Navigation Image Guided Surgery System | 7D Surgical - Image Guided Surgery
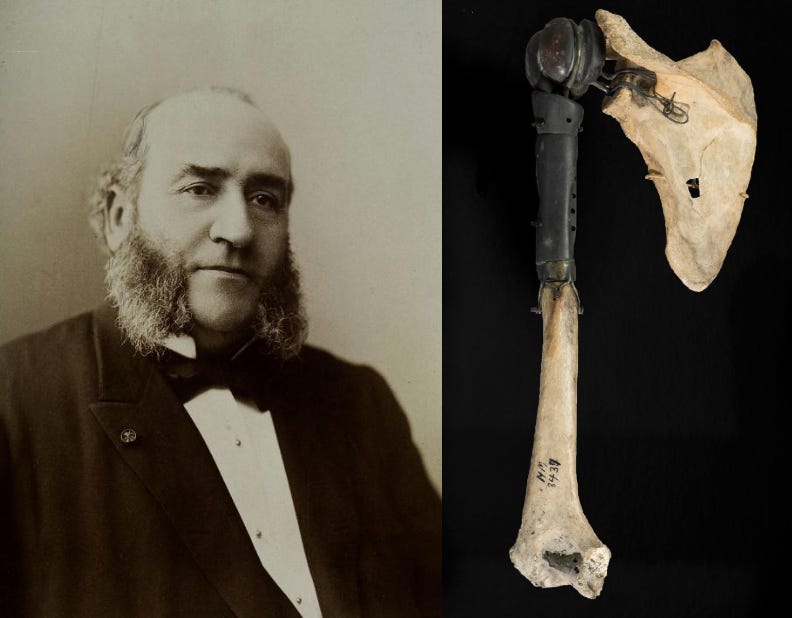
A curious case of curves #FromTheHistory:
Scoliosis is one of the oldest known deformities, described even in mythologies and studied since Hippocrates’ time. Of the many giants who embarked on finding a cure for the curves, was Jules Guerin. Inspired by Delpech and Stromeyer, Dr. Guerin proposed that scoliosis deformity is essentially due to deforming forces of muscles and myotomy would correct this. He went on to perform about 50 odd myotomies and tenotomies in each patient to correct scoliosis. Circa 1843, he published the results of 1349 patients declaring that 358 patients were completely cured of scoliosis.
Criticism of published literature was quite uncommon during those days. Dr. Malgaigne however, had some guts to break the custom. He pointed out the discrepancies in the statistics of the results and questioned the inferences of Dr. Guerin. Guerin took the fight to the next level. He sued Malgaigne for defamation.
Malgaigne described the suit as a “new simplification of orthopaedic discussions” and as a threat to the “free discussion of scientific affairs”. The case came to hearing before a large audience. Malgaigne pleaded himself and was able to win the case and its appeal.
And yes! he is the Malgaigne of Malgaigne fracture, the line of Malgaigne, Malgaigne amputation, Malgaigne Hook, and the triangle of Malgaigne.
“Scepticism is often the mother of understanding, of growth, and of perfection”

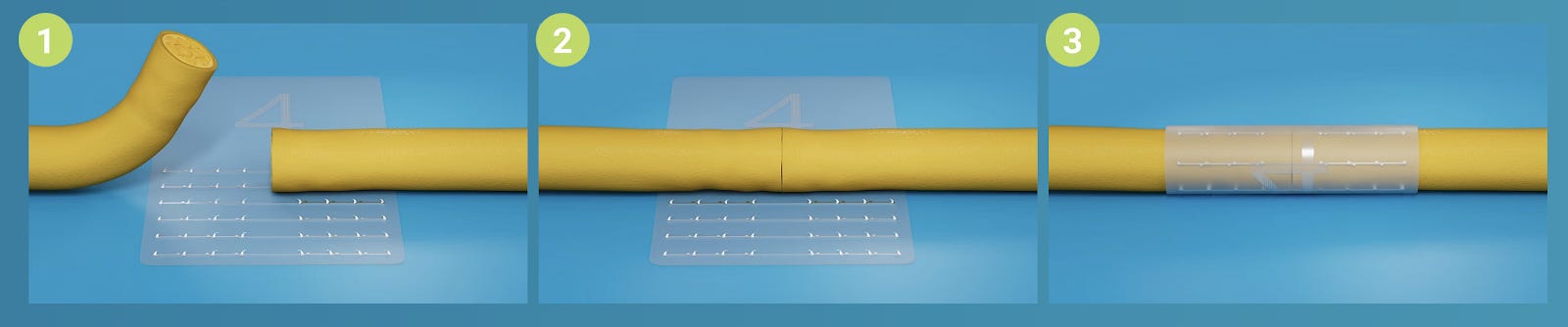
Sublamilar bands for a smooth transition - #SurgicalPearl:
Proximal junctional kyphosis (PJK) has a reported incidence of 17 to 62% and is seen as a harbinger of proximal junctional failure (PJF) in long-segment posterior spine fixations. An abrupt transition between the rigid, fused and flexible unfused vertebral segments has been attributed to the development of PJK. Sublaminar band construct at the proximal level is one trick to ensure a smooth transition to prevent PJK
• Through the midline posterior exposure, bilateral hemilaminotomies are done to widen the interlaminar spaces immediately proximal and distal to the UIV+1 laminas by using a power burr and Kerrison rongeurs. Avoid facet violation. The midline supra- and inter-spinous ligaments are also kept intact.
• The ligamentum flavum is removed using Kerrison rongeurs until the underlying dura mater is exposed.
• After ensuring sufficient hemilaminotomy windows, the 2 bands are sequentially introduced from the inferior to the superior end.
• Pressure over the dural sac during this manoeuvre is meticulously avoided.
• The tips of the bands are curved to prevent inadvertent impingement on the neural elements. At the level of the proximal hemilaminotomies, a nerve hook and/or a needle driver is used to gradually deliver the bands out.
• A sustained push is simultaneously applied with the other hand in a caudal-cephalad direction. The metal-backed tip of the band allows for its enhanced manoeuvrability during this process.
• It is better to do under motor and sensory neuromonitoring.
• After the bands are applied, pedicle screws are inserted at all thoracic, lumbar, and sacral levels as planned preoperatively. Rods are inserted bilaterally.
• Finally, the sublaminar bands are connected to the rods at the UIV level and hand-tensioned using a tensioner device.
• The decortication of bone is then performed, and the bone graft is placed up to the UIV level.


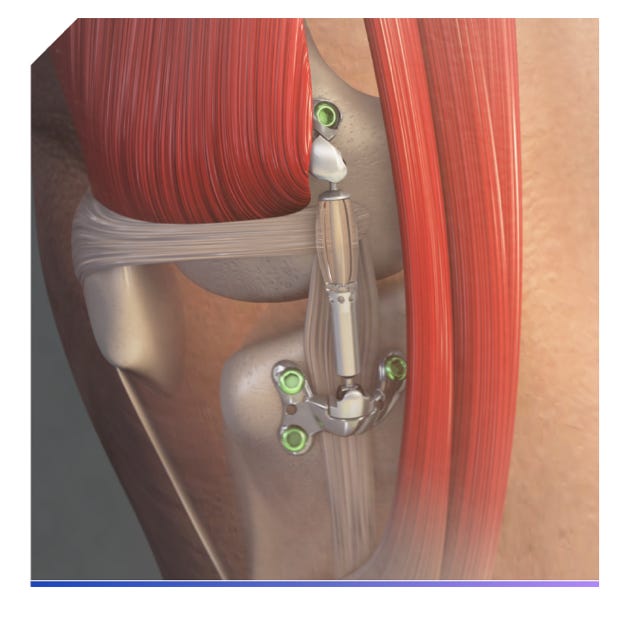
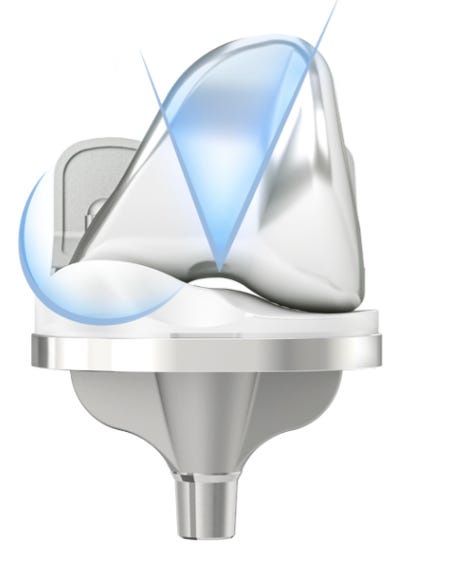
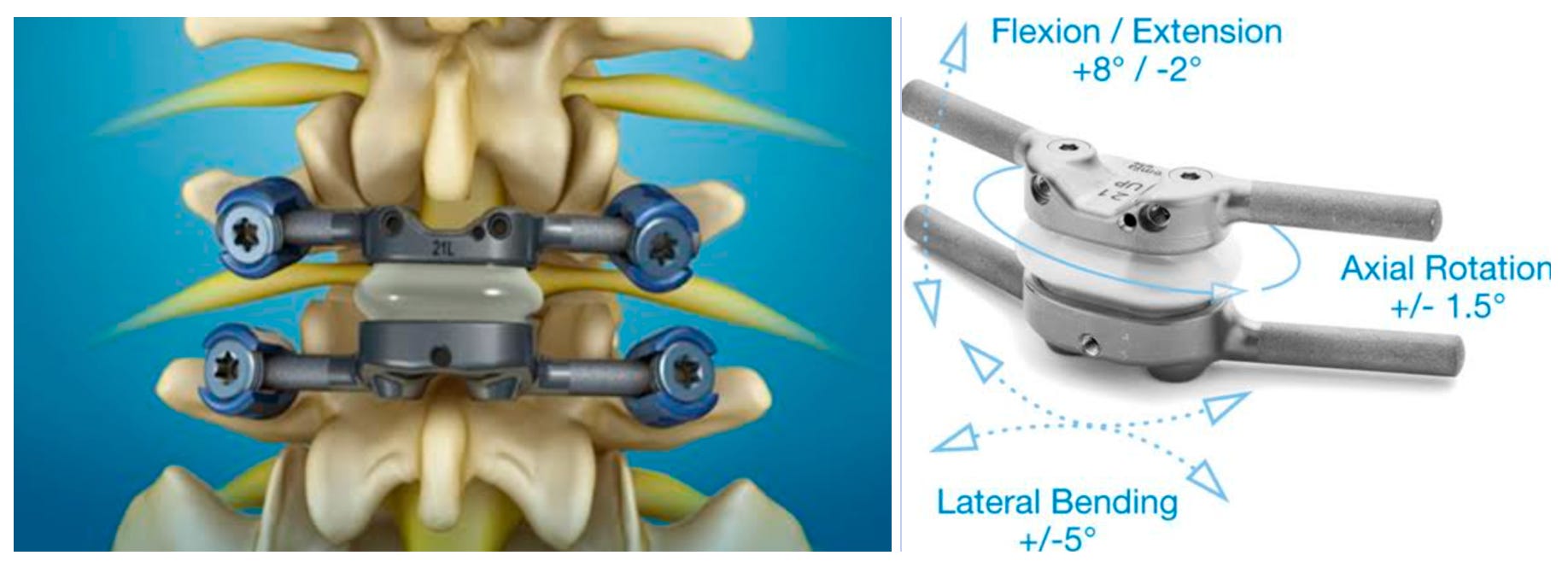
TOPS System seems to be at the top - #InTrials:
Though fusion has been proposed to be the ultimate solution for listheis, it is not without problems. Cries of the adjacent segment disease in long-term follow-up are getting louder day by day. Dynamic stabilisation systems were born out of these cries.
Total Posterior Spine System (TOPS) is one such system. To provide you guys with a headstart, it utilizes the pedicle screws and is comprised of two titanium plates linked by crossbars to screws on the same vertebra. This design curbs micro-motion and significantly reduces the risk of screw loosening. A key feature is the intervening capsule, crafted from a blend of titanium alloy and polycarbonate urethane, which replicates the function of natural facet joints. This enables controlled movement in multiple directions while restricting unwanted translation.
RCT by Domagoj Coric et al gives us proof of its safety and efficacy. The trial compared TOPS with transforaminal lumbar interbody fusion (TLIF) and pedicle screw fixation. in grade I listhesis. With a minimum follow-up of 24 months, the results are promising. The TOPS group exhibited a significantly higher overall clinical success rate (85%) compared to the TLIF group (64%). Notably, a greater percentage of TOPS patients (93%) experienced a ≥ 15-point ODI improvement compared to TLIF (81%).
Trivia: The FDA in June 2023 approved it for use in grade I degenerative spondylolisthesis.
MRI-based BMD is Reliable!!
Osteoporosis is a big menace. Quantitative CT-based bone mineral density (BMD) measurement has been the gold standard for identifying osteoporosis in spine patients. However, most spine patients end up only with an MRI. CT is done only in the setting of fracture. How good are MRI-based BMD assessment systems?
Kim et al. in their retrospective comparative study aimed to determine whether the MRI-based BMD scoring system on T1-weighted images can differentiate between healthy and osteoporotic vertebrae. They validated this scoring system against the gold standard CT measurements. The MRI-based system did differentiate between healthy and osteoporotic groups. ROC analysis revealed that a greater VBQ score was associated with the presence of osteoporosis. The cutoff VBQ for osteoporosis was 2.6.
Com’on guys! Quantify BMD on MRI for all degen. spine cases and start corrective measures.

Answer for the last month's question:
Which modality is more sensitive and specific to diagnose rotator cuff tears?
-
MRI
-
MR arthrogram
-
USG
According to a network meta-analysis by Liu et al of 144 diagnostic studies, MRA had the highest specificity and sensitivity followed by MRI and USG.
Upcoming events to check out:
-
21st ESSKA Congress 08-10 May 2024, Milan, Italy
-
61st Nordic Orthopaedic Federation (NOF) Congress 12 -14 June 2024, Netherlands
-
Orthopaedic Research Society 2024 Annual Meeting 2 - 6 February 2024, Long Beach, USA
Question of the month:
Which of the following add up to NEXUS criteria for C-Spine imaging in trauma?
-
Midline neck tenderness
-
Severe Injury in the lower limb of the patient
-
Altered consciousness of the patient
-
Breath smells of alcohol
Wait for our December issue to know the answer.
Have a marvellous month ahead folks!