Hawkins - a fusion puzzle of opposite poles!
Enjoy your brew with our exclusive issue on Foot & Ankle
Expedition to join the opposite poles. #NeoArmory:
We at BWB love polarizing opinions. It creates healthy debates and instils innovation. Occasionally, there comes someone who has the potential to unite both sides by combining their ideologies.
In the foot and ankle world, there are syndesmotic screws-ers or suspend-er?? Eh?
Paragon28, a Colorado-based foot and ankle implant makers have an R3ACTTM syndesmotic system in their showcase. It is a screw which gives the stability needed for ligament healing and on mobilising off the cast or boot, becomes a suspensory fixation by disengaging at the incisura - giving up to 3.5mm of diastatic mobility in all directions fixed by suture.

At 300,000 cycles, this is said to be better than the 2-suture construct as per performance analysis. Please do mind that there are no human studies available yet but this is something we will be out for with interest. Follow this space for updates.
If you've made it this far, look why they have the number '28' on their brand name
From Talus to Hand Surgery: #FromTheHistory:
It is rare to find someone who can publish, at the end of his orthopaedic residency, a landmark paper which changed the understanding of talus fracture management. It is highly uncommon for him to further his practice in Hand surgery and not in foot and ankle surgery.
Dr. Lenard Grene Hawkins walked through this unique career course for reasons not clear. A gifted student, Hawkins was inquisitive and shrewd enough to collect, collate, compile and publish the outcomes of talar fractures from 1943 to 1967 from the University of Iowa during his residency. He introduced the talar fracture classification system, which for the first time associated the development of avascular necrosis of talus to specific fracture types. He also described the reappearance of radiolucency in the subchondral talat region as a sign of revascularization. This sign famously called Hawkin’s sign was later extrapolated to other joints as well, helping us understand the importance of blood supply in bone turnover.
Despite all these landmark descriptions that shaped the management of talar fractures, Hawkins shifted his attention to upper limb surgeries after residency. His research works in the upper limb include bites on the hand, bier block in upper limb surgeries and complications of street drug injection into the upper limb.

Don’t miss this piece in the puzzle: #MostCited:
Many a time, ignored syndesmotic injury can be the missing piece in solving the puzzle of complex ankle fractures.
Lei et al. came out with preoperative CT parameters to prevent missing syndesmotic injuries. In their propensity-matched study, they concluded that the increased area of the syndesmotic joint and increased maximum tibiofibular distance at the level of syndesmosis are the two important diagnostic markers for syndesmotic injury.

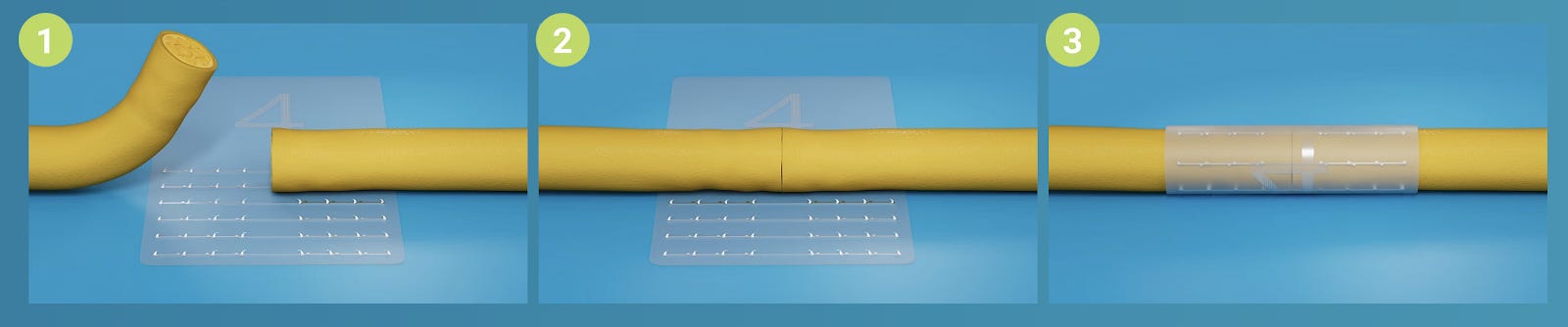
3 simple steps for calcaneus fixation #SurgicalPearl:
The phrase “Less is more than enough” holds good in some complex problems in Orthopaedics as well as life!
And Calcaneal fractures are one among them.
-
Patient in a prone position - the process of reduction consists of - distraction, elevation and clamping.
-
Distraction - using bilateral ankle distraction device - to restore the calcaneal height - pins are put in the distal tibia and calcaneal tuberosity. This also corrects the varus deformity.
-
Elevation - Joint depression fracture: Sanders type II - The reduction is achieved by percutaneously inserting a 2.5 mm K-wire into the de-pressed fragment from the plantar aspect.
-
In Joint depression fracture: Sanders type III and IV - More 2.5 mm K-wires are needed to be percutaneously inserted into each depressed fragment from the plantar or lateral wall.
-
In Tongue-type fracture: A 4 mm Steinmann pin is directed into the tongue-type fragment from calcaneal tuberosity through a 7 mm longitudinal incision lateral to the Achilles tendon. By levering the pin and mobilizing the fragment, the reduction may be achieved.
-
Clamping - to restore the calcaneal width - using a special clamp designed by the authors - medial calcaneal wall (beneath the tarsal tunnel) to the lateral side
-
Two 3.5 mm cannulated screws inserted transversely from the lateral wall to sustentaculum tali and a crossed fixation with two 5.0 mm craniocaudal fully-threaded screws are used to fix the fracture after provisional stabilisation with K wires.
Check out the full technique here
Fusion vs Fixation #InTrials:
Do you fix Lisfranc's injuries? Well, some fuse these primarily. Curious to know which modality fares better? Come let us dive into the RCT by Chengyi Sun et al.
In this trial, 78 cases of Lisfranc injuries with first TMT joint dislocation were analyzed. The participants, averaging 40.7 years, were divided into ORIF and primary fusion groups. 40 underwent ORIF and 38 underwent fusion, with a follow-up duration of 37.8 months (24-48 months). At the final follow-up, the ORIF group exhibited significantly lower scores in the AOFAS midfoot scale, FAAM Sports subscale, and the physical function and Bodily Pain scores of SF-36 (P < 0.01). The VAS score was higher in the ORIF group (P < 0.01). Redislocation of the first TMT joint occurred in ten ORIF cases, and thirteen patients reported midfoot pain. In contrast, no redislocations or hardware failures were reported in the fusion group.
The winner is the primary fusion guys!

Interesting events to check out:
-
21st ESSKA Congress 08-10 May 2024 Milan, Italy
-
Arthroscopy Association of North America (AANA)/ISAKOS Knee and Shoulder Course 5 - 6 April 2024 Florida, US
-
24th Annual Scientific Meeting - Asia Pacific Arthroplasty Society 21 -24 August 2024 Mumbai, India
Answer to previous month's question:
When to reconstruct the torn ACLs? What does the current evidence suggest?
-
Early
-
Delayed
-
Does not matter
Liu et al in their systematic review of 10 RCTs and 14 comparative studies conclude that reconstruction within 3 weeks is better i,e., early ACLR is better.
Question of the month:
In lateral malleolus fractures, are locking plates superior to non-locking plates?
Well, hold your curiosity till our next issue.
Have a marvellous March guys.