Be Ready For Office Jobs
Enjoy your Brew with this exclusive issue on Office Orthopaedics
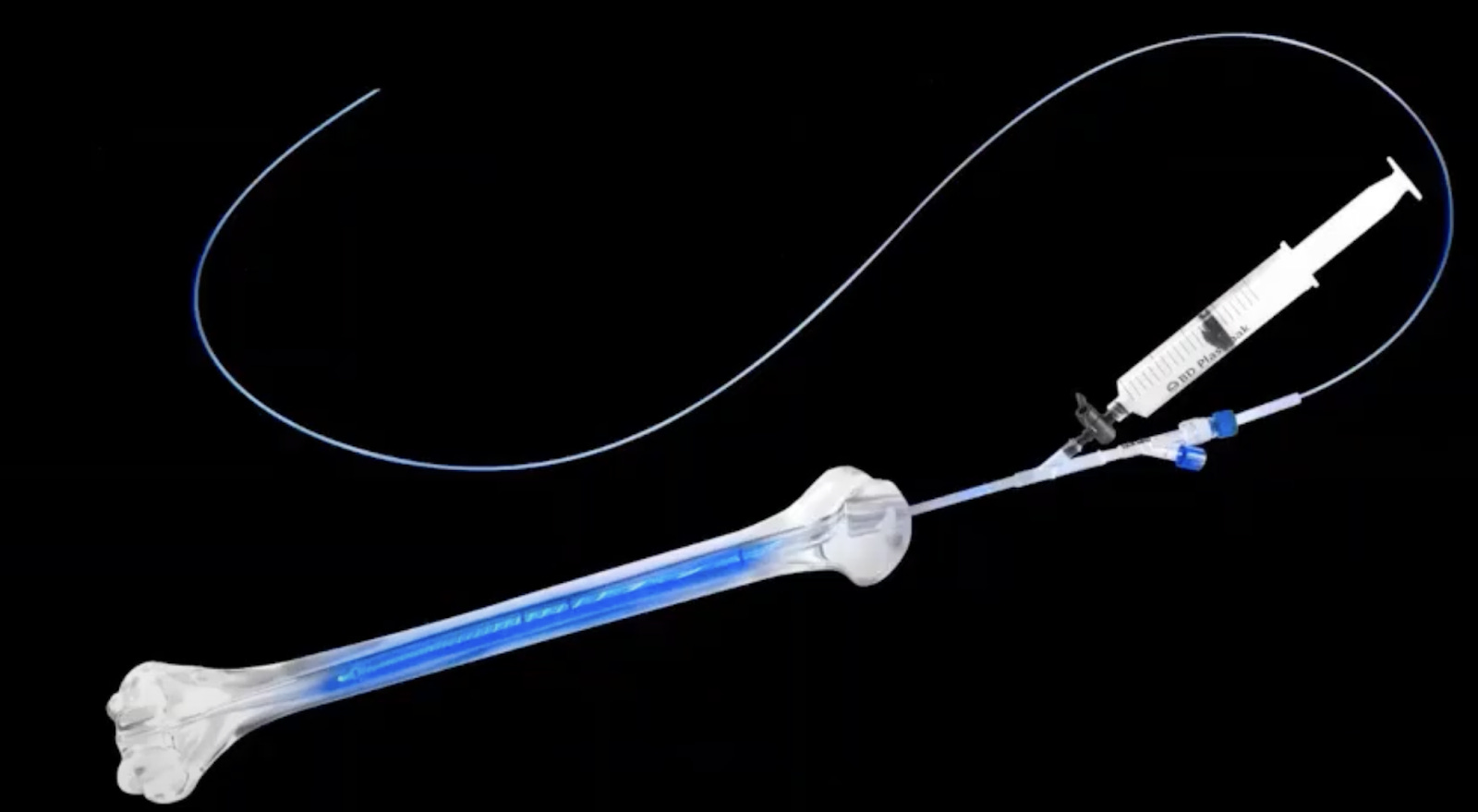
Nanobots? Nope. Just a Gel That Sticks Around for 5 Years
Where do sci-fi movies turn to when the plot is thrown into a corner? ‘Nanobots’. They inject something into the blood stream and the little ‘bots’ do all the work and create a superhero.

What if, we say that there is a similar injection similar to treat knee osteoarthritis! (Well, except for the nanobot part)(and the superhero part).
Contura Orthopaedics have created Arthrosamid a first “injectable synovial implant”. It a 2.5% PolyAcrylamide gel(iPAAG) which coats the synovial membrane and gives pain relief upto 5 years!

When injected, the compound integrates into the synovial membrane and remains as non biodegradable, non absorbable and non migratory, although we don’t yet know how the pain relief is achieved.
The compound itself is not new, been used up for soft tissue augmentation and bilking agent in stress incontinence almost for 40 years. Also, been injected into race horse knees with excellent effects.
This is not yet FDA approved but CE approved for use in Europe and being used in the UK and Canada. Does it cause any short or long term issues with knee replacement after injection? We don’t know yet.
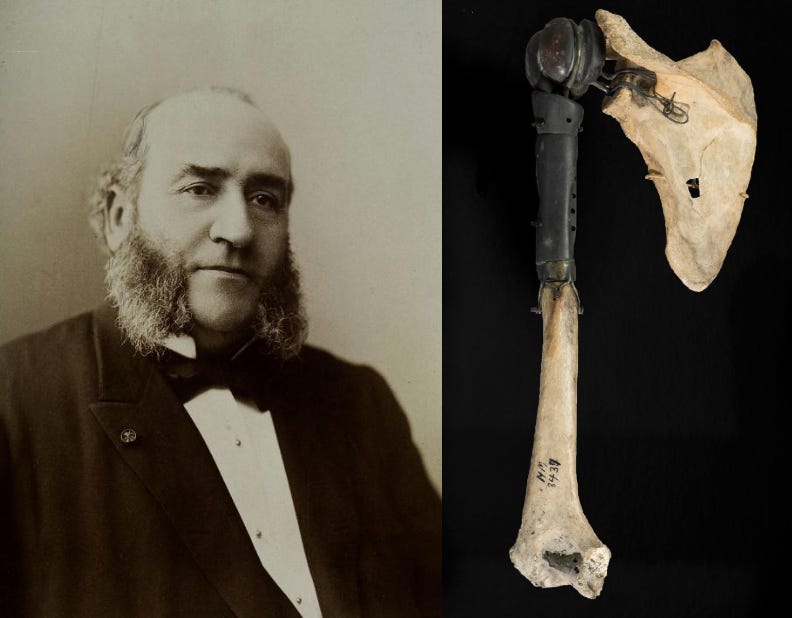
(Stetho)Scope in trauma - Ah! Come on! #FromTheHistory:
How did our forefathers identify and treat the not so easily identifiable fractures, without X rays? Did you ever wonder? It is not just before the discovery and introduction of X rays in the market, even after that, not every place was able to procure a machine. So, how did they manage, especially the ones like impacted neck of femur fractures?
Two words: Percussion and Auscultation!
Josef Leopold Auenbrugger (19 November 1722–17 May 1809) learnt this technique in the wine cellars of his father’s collection and used it to describe shoulder dislocation with percussion technique - Learnt the technique and brought it into his practice from a wine cellar, think about that! He taps on the olecranon process and immediate auscultation, viz., keeping his ear on the manubrium and hearing the conducted sound and it is called Auenbrugger sign and later became Heuter’s sign if you placed the bell of the stethoscope on the manubrium.
Rene Theophile Hyacinthe Laënnec (1781–1826) is the one we all know who invented the stethoscope. But do you know that he invented in order to avoid leaning on and hearing to the heart of a young lady with a heart condition? Yes, he wanted to avoid the awkward moment and at the same time he remembered some children playing with a wooden tube to amplify a sound and he thought can I do the same to hear the chest sounds and voila, we have a stethoscope. Though Laënnec didn’t write explicitly about using the stethoscope for identifying fractures, Jacques Lisfranc (12 April 1787–13 May 1847) wrote about the brilliance of Laënnec in identifying even those impacted neck of femur fractures, and even when patient is able to walk.
Finally, can you fathom that Kuntscher, Lipman and several other surgeons have just used percussion and auscultation not just to identify the fractures but also to understand if there was a good reduction and even placed intramedullary nails with closed technique without X rays!
No, X rays are needed, but when we don’t have them, take out that old stethoscope and dust it off and start using it.

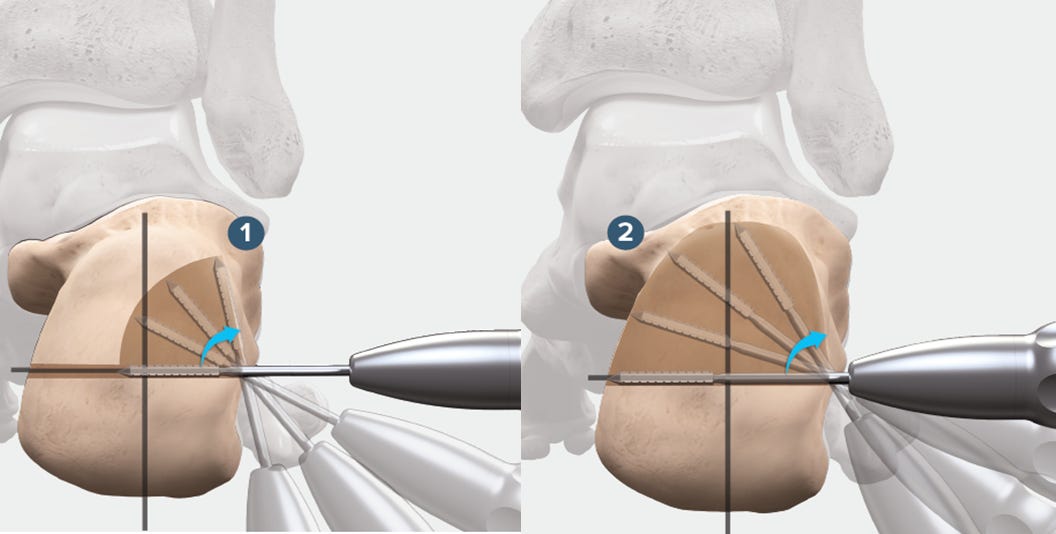
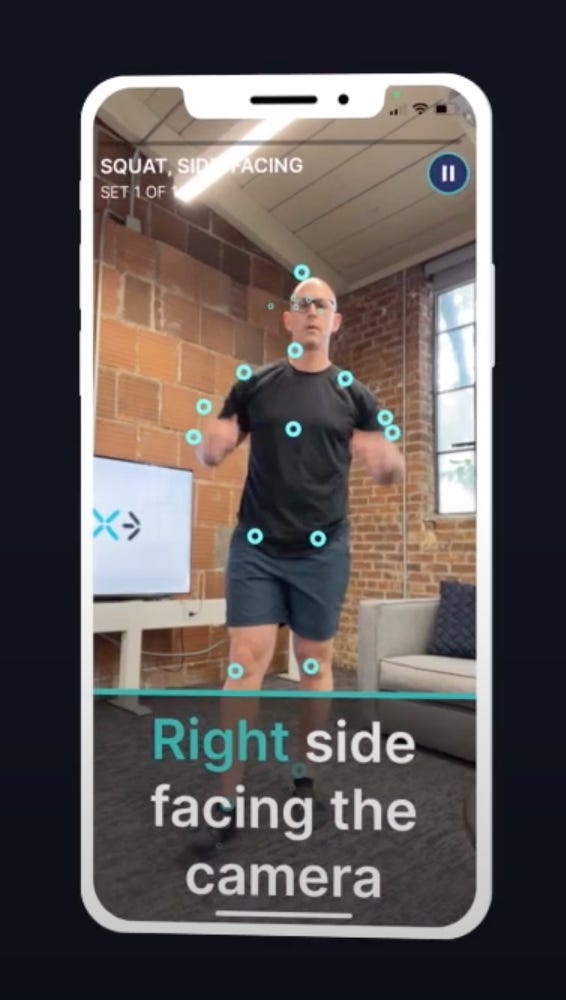
Genicular Nerve Radiofrequency Ablation (GNRFA) - #SurgicalPearl
Genicular Nerve Radiofrequency Ablation (GNRFA) is an outpatient pain procedure gaining ground in the treatment of moderate to severe knee osteoarthritis, especially in patients who’ve failed conservative treatments, had an unsatisfying knee replacement, or aren’t ideal surgical candidates.
Here’s how the technique works step-by-step:
-
Diagnostic Block: First, a test injection with 1 mL lidocaine is given near three sensory nerves—superior medial (SM), superior lateral (SL), and inferior medial (IM) genicular nerves. If pain relief >50% lasts 24 hours, the patient proceeds to ablation.
-
Positioning: Patient lies supine with 30° knee flexion. The knee is sterilized and draped. A ground pad is placed to avoid skin burns.
-
Landmark Identification:
-
SL nerve: Junction of femoral shaft and lateral epicondyle (AP view).
-
SM nerve: Just anterior to the adductor tubercle on the medial distal femur.
-
IM nerve: At the junction of the medial tibial metaphysis and diaphysis, along the tibial flare.
-
-
Cannula Insertion: 20G radiofrequency cannulas (3.5-inch, 10-mm active tip) are advanced percutaneously to contact bone at these landmarks under fluoroscopy.
-
Confirm Position: On lateral view, all cannulas should lie at the midpoint of the diaphysis. Adjust 3–5 mm if needed.
-
Nerve Testing: Sensory testing at 50 Hz reproduces typical pain. Motor testing (2 Hz) confirms no motor involvement.
-
Ablation: Each site is injected with lidocaine, then ablated at 80°C for 90 seconds. Cannulas are advanced slightly, and ablation is repeated.
-
Steroid Injection & Wrap-Up: 1 mL methylprednisolone is given post-lesion. Cannulas removed, sites bandaged.
The result? Months of relief for patients with limited options—no incision, no implant, and no general anaesthesia required. Read the detailed description of the technique here.

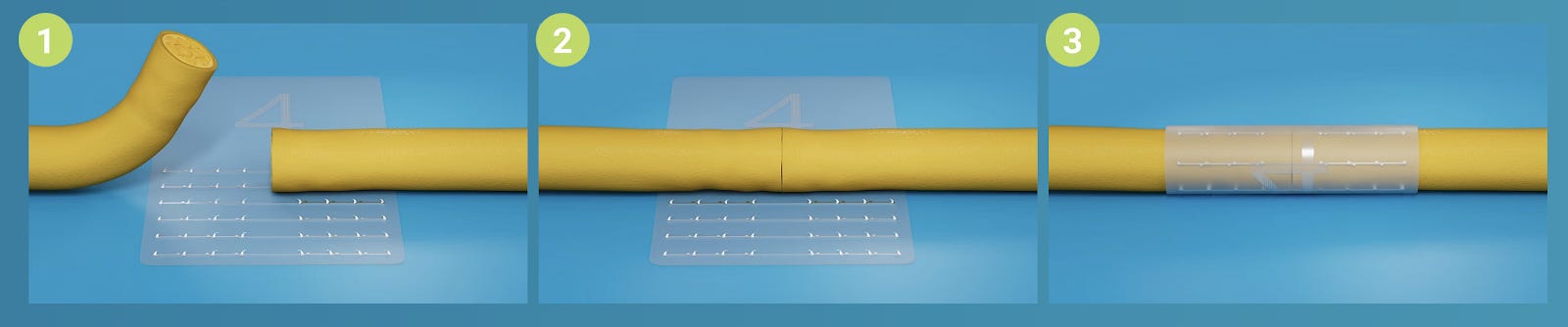
???? Big Dose or Small Dose? Turns Out, It Doesn’t Matter Much for CTS
Carpal Tunnel Syndrome (CTS) is one of those sneaky little conditions that can really mess with daily life—and steroid injections are often the go-to relief plan. But how much steroid is really needed? A recent randomized controlled trial put that exact question to the test.
Researchers compared 10 mg vs. 40 mg doses of triamcinolone acetonide (TA)—both mixed with lidocaine—given under ultrasound guidance for patients with mild to moderate CTS. Over 12 weeks, they tracked pain levels, symptoms, function, and even nerve conduction studies. Spoiler: both groups did equally well across the board.
So what’s the takeaway? You can likely get the same bang for your buck—and symptom relief—with just 10 mg of steroid. That means less drug, potentially fewer side effects, and more cost-effective care. It’s a win for patients and a win for resource-conscious clinicians.
This study reinforces the idea that in medicine, more isn’t always better. Sometimes, keeping it minimal does the job just fine.

Ponseti’s Clubfoot Protocol: Tenotomy Timing Makes the Difference
In the stiff clubfoot game, timing is everything, especially when it comes to Achilles tenotomy. So, should we snip sooner rather than later?
A randomised trial by Ghanem et al. put the method to the test: 140 stiff feet, split evenly into early and late tenotomy groups, all treated with the Ponseti method. The verdict? Early tenotomy at the first cast not only reduced technical hiccups (just 3% vs. 38%), but also scored better long-term outcomes — more “excellent” feet and fewer talar dome issues.
Why does it work? Easier access to the tendon on an untouched foot and less joint compression after an early release appear to provide both surgeons and neonates a smoother experience.
Moral of the story: If you’re in the early intervention camp, science is backing you — early may just be the new gold standard.
Events to watch out:
-
Ranawat Orthopaedic Conference (ROC 2026) 08 – 10th Jan 2026 - Bengaluru, India
-
Global Knee Innovation Summit 22 – 24th Jan 2026 - Dubai, UAE
-
Asia Pacific Orthopaedic Association (APOA) 25th Congress 04 – 07th Feb 2026 - Jaipur, India
Answer to last month question:
Which bone sarcoma subtype had the highest pooled 5‑year overall survival rate?
A. Chondrosarcoma
B. Ewing’s sarcoma
C. Osteosarcoma
D. Metastasis
Answer: Ewing’s sarcoma according to a systematic review by Hosseini et al.
Have a fabulous month ahead guys!